Introduction
There has been increase in the treatment modalities for non-surgical Class II malocclusion.
This has resulted in orthodontists becoming more vigilant with extraction treatment plans and exploring possible non-extraction treatment approaches. Maxillary molar distalization is one such method. The maxillary molar is distalized to create space and helps in solving the malocclusion. The treatment of Class II malocclusion depends on patient age, patient facial appearance, likely stability of overjet reduction, and whether it is skeletal or dental. It can be treated by growth modifications, orthodontic camouflage, or surgical correction. Class II relationship without extraction is treated by distal movement of maxillary dentition, mesial movement of the mandibular dentition, or an amalgamation of both. Distal movement of maxillary molars is frequently required in treating of Class II malocclusions without extractions. Hilgers in 1992 introduced the pendulum appliance which became popular and was widely used to create space and gradually many other appliances were developed for the distal driving.1, 2 Both intra-oral and extra-oral methods are present. The extra oral appliance includes headgear and heavy elastics; whereas intra oral appliance include distal jet, jones jigs, pendulum appliance, k-loop, fixed functional appliances, magnets, ACCO appliance and use of TAD’s.
Case Report
Section I: Pre-treatment assessment
History and clinical assessment
P.K a 14 year 2 months old female came with a chief complaint of irregularly placed upper and lower front teeth region. Patient had undergone root canal treatment i.r.t 46 and had prosthesis for the same. No other significant medical and dental history were present.
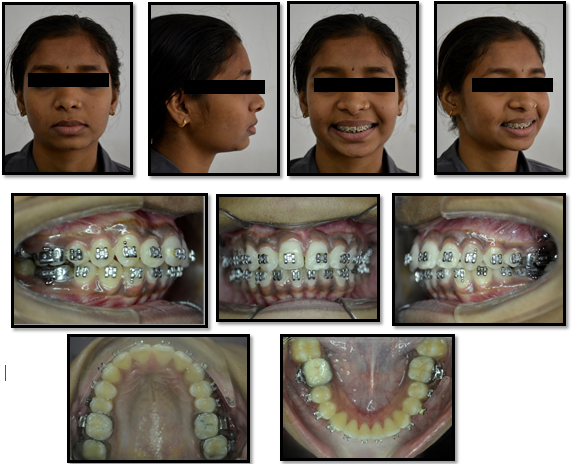
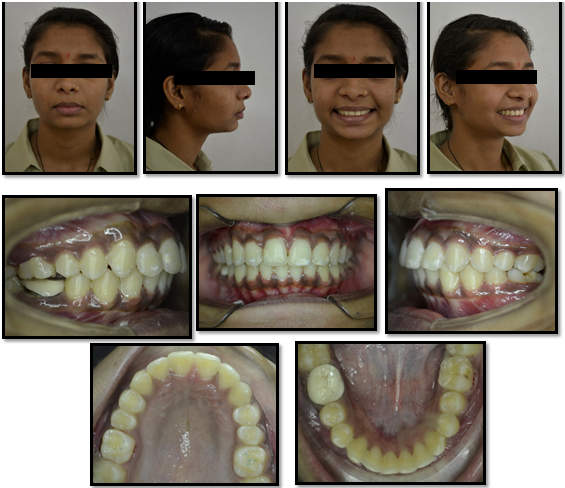
Extra-oral examination (Figure 1) revealed mesoprosopic facial pattern, with convex profile and competent lips, nasolabial angle and mentolabial sulcus appeared to be normal. Lips appeared to be normal. Functional analysis showed a normal temporomandibular joint.
Intra-oral examination (Figure 2) showed permanent dentition with Angle’s Class 2 subdivision on left side and Class 1 molar relation on right side; and Class 1 canine relation on right and end on canine relation on left side; and incisor relation of Class II div I with overjet of 4.5mm and overbite of 3mm was seen. Upper midline was shifted to right by 0.5mm and lower midline shifted to right by 2mm. Crowding was present in upper and lower anterior region.
General radiographic examination
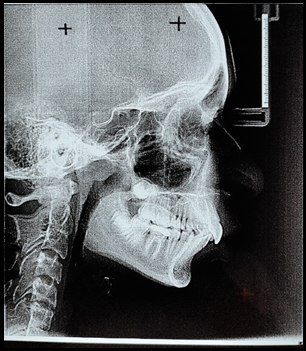
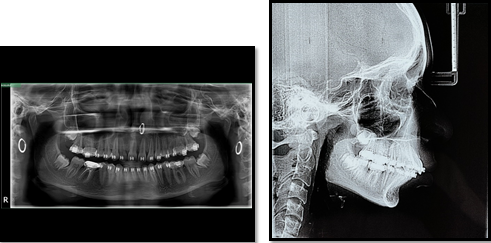
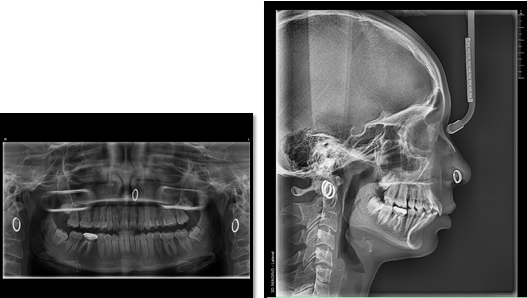
Pre-treatment panoramic (Figure 3) Lateral cephalogram (Figure 4) were recorded and various analysis were done.
Panoramic radiograph revealed symmetric dental development on both the sides. All the permanent teeth and developing tooth germs of all the third molars were present. The alveolar bone levels and root morphologies of the teeth were normal. Temporomandibular joint space appeared optimal with normal size, shape, and position of condyle heads. Root canal treatment was done in 46 and had prosthesis for the same.
Cephalometric analysis (Table 1) shows Class I skeletal pattern, with convex profile, proclined upper and lower incisors, horizontal growth pattern; increased overjet and overbite. CVMI stages showed completion of growth.
Diagnosis and etiology
P.K a 14-year-old female patient presented with Angle’s Class II subdivision superimposed on Class I skeletal jaw bases with Class II molar relation on left side and Class I molar relation on right side with end on canine relation on left side and Class I canine on right side along with Class II div I incisor relation with a horizontal growth pattern, upper and lower incisor proclination, increased overjet and overbite, crowding in upper and lower arch, convex profile. Probable aetiology may be early loss of maxillary deciduous posteriors leading to mesial movement of the maxillary permanent teeth.
Treatment objective
To achieve Angle’s Class I molar relation on the Left Side.
To achieve Ideal Class I canine relations on Left side.
To maintain Class I molar and canine relation on Right side.
To achieve ideal inclinations of U/L anterior teeth.
To achieve Ideal Overjet and Overbite.
To resolve crowding of teeth.
To correct rotations of individual teeth.
Treatment plan
The treatment plan for the patient was en-masse unilateral distalization of buccal segment on left side with IZC implant. Initial leveling and aligning of the teeth were done with 0.022MBT appliance. Once the aligning was done and 0.019*0.025 SS wire was reached IZC (Infra-zygomatic crest) implant of size 2*12 mm was placed in crest of zygomatic bone for better anchorage control due to increased bone density. 3, 4, 5 After distalization indirect anchorage from the implant was taken to maintain the class I molar and canine. Finishing and detailing was done later on.
Section II: Leveling and Aligning / Pre-Distalization Stage
The bonding of all teeth were done with 3M unitek metal brackets and all the molars and 2nd molar of upper arch were banded. The wire sequence was progressed according to the MBT. Once the 0.019*0.025 SS stage was reached; pre-distalization records were taken. All the photographs (Figure 5), radiographs (Figure 6 ) were taken and patient was prepared for IZC implant insertion.
Section III: Placement of IZC Implant
Infra-zygomatic crest implant was placed distal to 26 on the crest of zygomatic bone. Initial placement was done at 90 degrees and slowly tilted to 60 degrees.6
After the implant was placed Ni-Ti coil spring was used to distalize. A power arm was attached mesial to canine for the attachment of coil spring. The opposite arch was tightly consolidated and cinch back was done to prevent unnecessary space opening. The coil spring extended from the implant to the top hook of the power arm to allow unilateral en-masse distalization of the left side. The patient was re-evaluated every 4 weeks. 7, 8
Section IV: Post distalization stage
After 6 months of distalization with Ni-Ti coil spring; the molars and canine were achieved in Class I relation. Unilateral en-masse distalization on left side was done. There was decrease in the overjet, the overbite was also reduced. Minor spaces were opened and were closed with e-chain. The midline shift was also noticed which lead to coinciding upper and lower midlines.
There was reduction in the upper and lower proclination. Marked improvement in the soft tissue and profile change was seen.
Section V: Post treatment stage
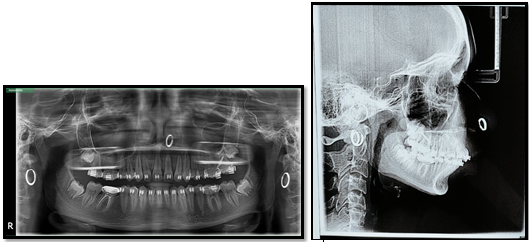
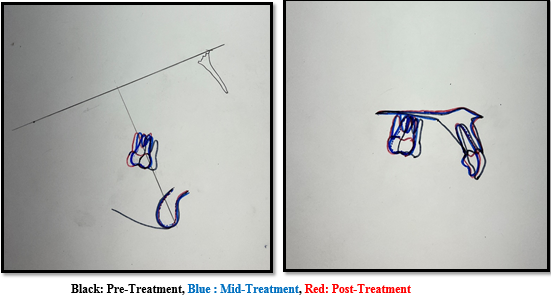
After finishing and detailing and proper interdigitation the patient was debonded. Post treatment photographs (Figure 11) showed full cusp class 1 molar relation bilaterally, class 1 canine relation bilaterally, relieving of crowding in both the arches, coinciding midlines, ideal overjet and overbite was achieved.9 There was marked improvement in the soft tissue parameters, increase in lower anterior facial height, improvement of the convex profile, and ideal nasolabial sulcus, all these results were supported with post-treatment radiographs (Figure 12). Cephalometric superimposition (Figure 13) showed distalization of upper molar along with reduced upper and lower incisor inclination. Upper and lower removable hawley’s appliance was given to wear for full time as a retention protocol.10
Discussion
Infra-Zygomatic crest implants and Buccal Shelf implants have been a great boon to the field of orthodontics. The IZC and BS region are considered the safer zone as these areas are devoid of important anatomical structures like a tooth root or nerves. The absence of hindrance to the roots of teeth allows for more versatility of Orthodontic tooth movement. Another advantage is the primary stability. It is defined as the absence of mobility in the bone bed after mini-screws placement. It is dependent on how bone screws engage mechanically the bony region while and after driving into the bone. IZC/BS regions have good quality and quantity of the bone to provide good primary stability. Bone density is also high with D1 >1250 HU. One the other major advantage is biomechanical ability to provide translation or bodily movement for the distalization of molar; as the force passes through the centre of resistance in the form of ni-ti coil spring and the length of the power arm. Thus avoiding the distal tipping of the molar. Unlike other appliance IZC implants appears to be better choice in terms of patient compliance, tooth movement and activation. In comparison with other appliance like pendulum appliance or jones jigs or distal jet, more translatory movement is achieved in the fistulizing with IZC rather than distal tipping of the molar. In this case IZC implant was chosen as method for distal driving of the molar because en-masse distalization was needed and tipping of molar couldn’t have solved the problem. This also helped in reducing the upper and lower anterior proclination. On cephalometric analysis when the perpendicular vertical was drawn from Ptm i.e ptv to measure how much molar was distalized. Distalization of 4mm was achieved with the help of IZC implant. 11
Critical Appraisal
P.K had class II division I subdivision on left side, with class I skeletal jaw bases, upper and lower crowding and convex profile. Careful insertion of IZC implant was done and unilateral en-masse distalization on left side was achieved. The post-treatment results achieved were highly satisfactory with good posterior occlusion and excellent facial soft tissue balance and harmony. The patient and parents were highly satisfied with the treatment result. The use of non-extraction treatment approach such as molar distalization, helped in avoiding over‑retraction of maxillary incisors and dishing in the patient’s profile. Lower anterior facial height also improved which helped in overall aesthetic improvement. Post-treatment class 1 molar and class 1 canine was achieved with coinciding midlines, and improved profile. Post-treatment panoramic radiograph showed good root parallelism which will ensure good stability of the results achieved. The patient was advised that the un-erupted third molar in the may warrant extraction at a later date.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.