- Visibility 117 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijodr.2021.046
-
CrossMark
- Citation
A review on open bite
- Author Details:
-
Anshul Munjal *
-
Adeeba Ali
-
Sharon Ann Abraham
-
Bater Jini
Introduction
Any increase or decrease in vertical dimension of face results to vertical dysplasia. The increased vertical dimension can lead to OPEN BITE. The term “open bite” was coined by Caravelli in 1842 as a distinct classification of malocclusion [1] and can be defined in different manners.
Subtelney and Sakuda [2] defined open bite as an open vertical dimension between the incisal edges of the maxillary and mandibular anterior teeth, although loss of vertical dental contact can occur between the anterior or the posterior segment.

Prevalance
An open bite of greater than 2 mm occurs in less than 1% of the population and has five times greater prevalence in the black population than in the white or Hispanic populations.[3] The incidence of anterior open bite ranges from 1.5% to 11% [4] and varies between races and with dental age.[5] In the mixed dentition the prevalence of the anterior open bite can reach up to 18.5%, decreasing with age.
Classification
Worms, Meskin and Isaacson[6] provided classification based upon clinical findings:Simple OB: from canine to canineCompound OB: from premolar to premolarInfantile OB: from molar to molar
According to Proffit, [7]Open bite (mm) >-4 extreme -3 to -4 severe 0 to -2 moderate
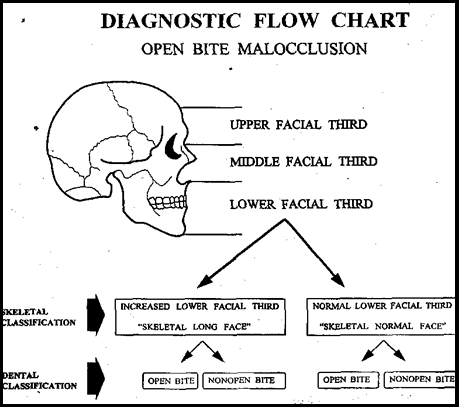
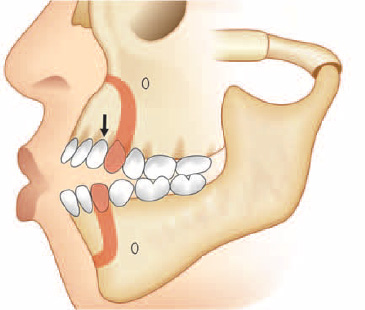
Sassouni [8] classified open bite by taking mandibular plane angle into consideration as ([Figure 2]):
Skeletal open bite
Dentoalveolar open bite
Based on 1st molar antero-postero relationship
Class I
Class II
Class III
Rakosi [9] classified open bite based on tongue posture as ([Figure 3]):
Anterior open bite-Open bite in a deciduous dentition, caused by tongue dysfunction as a residuum of a sucking habit.
Lateral open bite-Occlusion, in this type of open bite on both sides is supported only anteriorly and by first permanent molars.
Complex open bite-Severe vertical malocclusion. The teeth occlude only on second molars.
Tongue dysfunction and malocclusion-in mandibular prognathism, the downward forward displacement of tongue often causes an anterior tongue thrust habit.
Etiology
The etiologic factors of open bite can be broadly classified into
Epigenetic factors
Environmental factors
Epigenetic factors
Posture, morphology and size of the tongue,
Skeletal growth pattern of maxilla and Mandible
Vertical relationship of Jaw bases
These characteristics are genetically determined.
Environmental factors
Thumb and digit sucking habit
The severity of malocclusion caused by thumb Sucking depends upon
Duration
Frequency
Intensity
According to Freud’s psychoanalytical theory, [10] all developmentally normal children possesses an inherent, biological drive for sucking. Rooting and placing reflexes are merely expressions of this drive. Environmental factors contribute transfer of this sucking habit to non-nutritive sources such as thumb or finger.
The effects of thumb sucking are;
Proclination of maxillary anteriors
Anterior open bite with supra-eruption of the buccal teeth
Leads to tongue thrust habit because of open bite
Upper lip is hypotonic and hyperactive mentalis activity.
Tongue thrust habit
According to Bahr and Holt, [11] the tongue thrust activity are classified into
Tongue thrust without deformation
Tongue thrust causing anterior deformation with an anterior open bite termed as simple open bite
Tongue thrust causing buccal segment deformation with a posterior open bite (Lateral tongue thrust activity)
Combined tongue thrust, causing both anterior and posterior open bite called complex open bite
Tulley suggested tongue thrusting as an endogenous habit or is an adaptive behaviour based largely on facial morphology and swallowing activity.
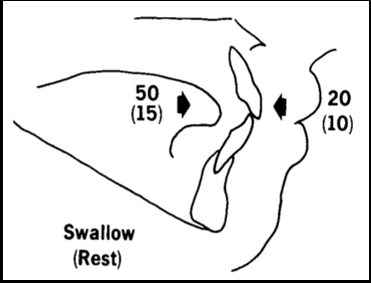
According to Proffit and Mason, tongue thrust is more likely to be an adaptation to the open bite, and therapy aimed at changing the swallowing pattern is not indicated. Given the physiology of tooth movement, it is unlikely that tongue thrust, but rather resting tongue posture, plays a role in the etiology of open bite
Equilibrium theory [12] ([Figure 4]) suggests that light continuous forces are responsible for tooth movement and position. These forces can be external (digits) or internal (tongue posture or periodontal forces). Abrupt, intermittent forces (tongue forces due to swallowing) are much less likely to be a causative factor. Proffit and suggest that therapy for anterior tongue position is not warranted with or without malocclusion before adolescence. Further, tongue therapy is most effective when combined with orthodontic treatment. Speech therapy may be combined with orthodontic treatment and possibly myofunctional therapy in older children.
Mouth breathing
It is the pattern of breathing totally/partially though oral cavity due to anatomical or functional variation. It can be classified as: Obstructive, Habitual and Anatomical.
When a person breathe through mouth, the mandible and the tongue are lowered, and the head is extended, if these postural changes are to be maintained, the vertical equilibrium will be disrupted causing over eruption of the posterior teeth, increase in lower facial height and change in cranio-vertebral angle by 5 degrees, which further leads to backward rotation of mandible and thus open bite. [2]
Clinical features are:
Long and narrow face
Narrow nose and nasal passage
Short and flaccid upper lip
Contracted upper arch
Flaring of the Incisors
Anterior marginal gingivitis due to drying of the gingiva.
Diagnosis
The diagnosis and treatment planning for open bite continues to be one of the most challenging situations facing Orthodontists today.
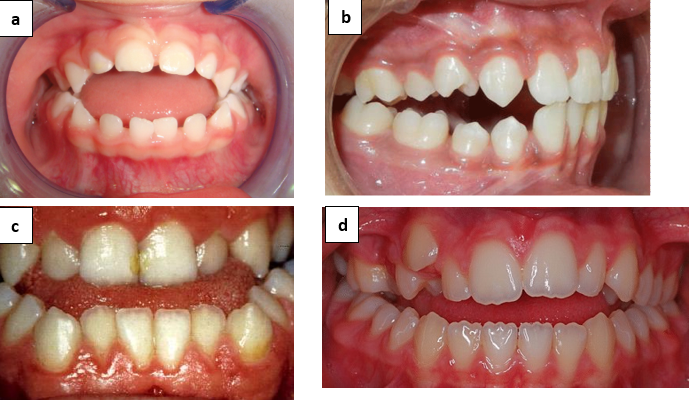
Clinically[13]
Overjet combined with an open bite less than 1 mm - Pseudo open bite
Open bite more than 1mm between the incisors, and posterior teeth are in occlusion - simple open bite.
Open bite extending from premolars (or) deciduous molars on one side to the corresponding teeth on the other side - complex open bite.
Compound (or infantile open bite is completely open including molars
Iatrogenic open bite is the consequence of orthodontic therapy. In mixed dentition, various therapeutic measures may cause open-bite.
An open activator with a high construction bite causes tongue thrust habit and results in anterior open bite. Intrusion of posterior teeth creates posterior open bite especially in deciduous molar area.
Expansion treatment - buccal segments tip buccally with elongation of lingual cusps. This creates prematurity and opens the bite.
In distalization of maxillary first molar with extra-oral force the molars are often tipped down and back, elongating the mesial cusps. This creates open bite in downward, backward growing faces with already having excessive anterior face heights.
Cephalometrically [13]
Dentaloalveolar open bite- Depends on the extent of the eruption of teeth. Supraocclusion of molars and infra-occlusion of incisors.
Lateral open bite- It is Purely dentoalveolar with infraocclusion of molars. Etiology can be cheek sucking, lateral tongue thrust or lateral tongue posture in postural rest position.
Skeletal open bite- There will be excessive anterior face height particularly lower third, posterior facial height will be short.
Mandibular base- is usually normal and antegonal notching is often present, symphysis is narrow and long, ramus is short, gonial angle is large and growth pattern is vertical.
Maxillary base- Vertical growth pattern:
Upward tipping of the forward end of the max base.
Downward tipping of the posterior end of the max base.
Horizontal growth patterns
Upward and forward tipping of the max base
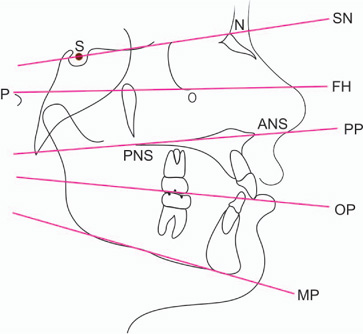
David and Richard Smith, 1998, has described the cephalometric and clinical diagnosis of open-bite tendency.
Steep mandibular plane angle
SN: MP angle 40° (or) greater
OP: MP angle 22° (or) greater
PP: MP 32° (or) greater
PFH/AFH ratio 58% (or) less
UFH/LFH Ratio 0 700 (or) less
Sassouni analysis
Sassouni [14] pointed out that the horizontal anatomic planes ([Figure 5]) -
The inclination of the anterior cranial base,
Frankfort plane,
Palatal plane,
Occlusal plane,
Mandibular plane-tend to converge toward a single point in well-proportioned faces.
The inclination of these planes to each other reflects the vertical proportionality of the face. If the planes intersect relatively close to the face and diverge quickly as they pass anteriorly, the facial proportions are long anteriorly and short posteriorly, which predisposes the individual to an open bite malocclusion (skeletal open bite).
If the planes are nearly parallel, so that they converge far behind the face and diverge only slowly as they pass anteriorly, there is a skeletal predisposition to anterior deep bite (skeletal deep bite).
Treatment plan
Treatment plan in deciduous dentition
No treatment up to 3 years of age
Dental type: Screening therapy
Skeletal type: habit control to reduce the increasing severity of dysplasia and the extra-oral orthopaedic appliances can be used effectively to redirect the growth (e.g.) chin caps
Treatment plan in mixed dentition
Early mixed dentition- Screening therapy
Late mixed dentition- Habit breaking appliance ([Figure 6])-Orthopaedic approach-Orthodontic approach-Myotherapy
**surgical resection of mentalis muscle is done in mixed dentition stage to decrease the golf ball chin effect.

Treatment plan in permanent dentition
Functional appliances
Fixed mechanotherapy
Surgery
According to Issacson and Worms, spontaneous correction occurs in 80 percent of mixed dentition cases. [15] Parker and Johnson (1993) suggested interceptive treatment to be carried out in cases that do not self-correct. [16]
Altering mode of breathing
Myotherapy
Habit breaking appliances
Functional orthopaedic appliances
Fixed mechanotherapy
Treatment modalities
Altering Mode of Breathing [17]Woodside confirmed that the change in mouth open breathing to mouth closed breathing reverses symptoms.
Tongue and mandible position raised
Increased width of maxillary arch
Increased depth of bony nasopharynx
Decreased lower facial height.
Myotherapy
Ask the patient to hold the piece of paper between lips
Practice swallowing pattern: placing tip of tongue on the palate, close teeth, close lips, and swallow with tongue in that position.
Clenching exercises- 15 seconds- 5 times a day[Figure 7]):
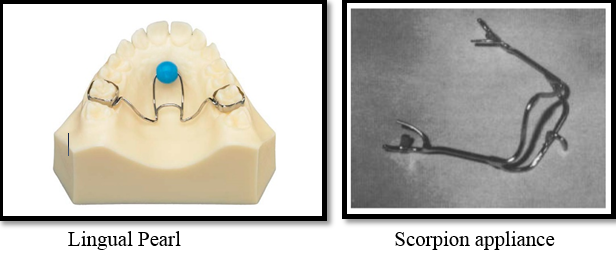
Lingual pearl (JCO 1998) [18]
Scorpion appliance [19]
Blue grass appliance
Habit Breaking Appliances
Tongue Crib Appliance – inhibitory appliance.
Vestibular screens- It is effective in eliminating the mouth breathing habit, abnormal sucking habits and lip dysfunction to achieve a proper lip seal, which is of prime importance. This lip seal will indirectly influence the posture of the tongue and thereby leading to maturation of the deglutation cycle and creates a somatic swallowing pattern. The appliance is usually worn at night and 2 to 3 hours per day
Functional Appliances
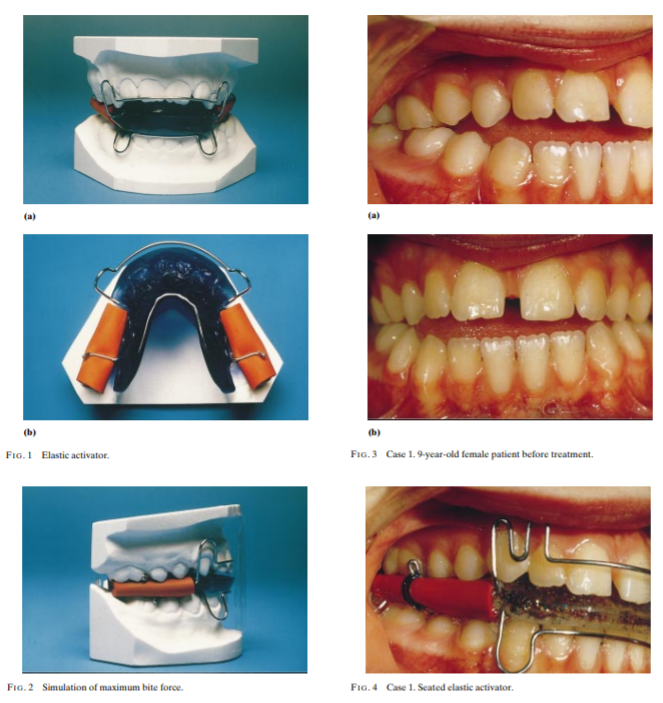
Activator- Stellzig et.al, 1999 has described about the ELASTICACTIVATOR for the treatment of open bite. [20] The intermaxillary acrylic of the lateral occlusal zones is replaced by elastic rubber tubes. By stimulating orthopaedic gymnastics (chewing gum effects) the elastic activator intrudes upper and lower posterior teeth. It also produces counter clock wise rotation of the mandible by decreasing the gonial angle ([Figure 8]).
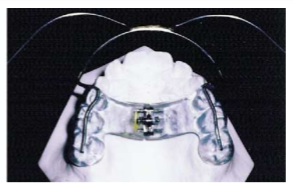
Functional regulator 4 appliance (FR4): Rolf Fränkel believe that correction of the faulty postural activity of the orofacial musculature might help correct the associated skeletal deformity, so he used FR4 appliance (conjunction with lip seal training to achieve over bite correction and elimination of the skeletal dysplasia 1980) ([Figure 9]). A randomized clinical trial conducted by Erbay et al. (1995) reported that the growth direction of the mandible could be changed to an upward and forward direction by FR4 therapy
TWIN BLOCK - In treating the patients with vertical growth pattern associated with anterior open bite and increased lower facial height, the contact between the occlusal bite blocks and the posterior teeth should be maintained to prevent the eruption of the posterior teeth.
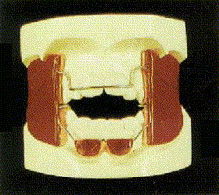
Modified Thurow appliance -: This modified appliance has acrylic occlusal splint and an expansion screw, which guides the vertical force against the posterior teeth and the alveolar process (Stuani, 2005). [21] An expansion screw in palate is incorporated to prevent and treat a posterior bilateral crossbite during the use of this appliance.
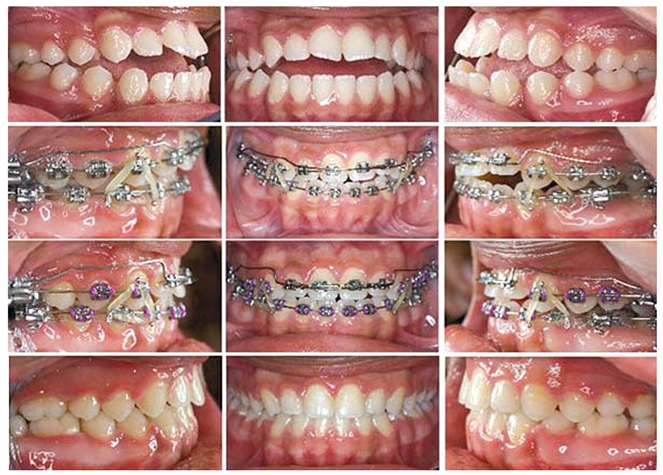
Fixed appliance treatment
Correction of open bite by incisor extrusion:
Vertical elastics [22] (Nanda, 2012) Indication:
Complaint patients
Patients with divergence of occlusal planes anteriorly. [Figure 11]).Poor control of the force magnitude and degrees in compliance are main inherent problems.
Extrusion arches
Noncompliant patients who will not wear anterior vertical elastics
When upper and lower occlusal planes that diverge anterior to the first premolars.
When a constant extrusive force is desired in the anterior teeth with minimal posterior side effects
Multiloop edgewise archwire (MEAW): Kim, (1987) developed MEAW consists of a 0.016”x0.022” stainless wire which contains a series of loops with both a horizontal and vertical component. [23]

Magnets
The use of a magnetic appliance in the treatment of skeletal open bite malocclusion was first illustrated in the literature in 1986 by Dellinger. His ‘Active Vertical Corrector’ consists of TWO removable bite block appliances (maxillary and mandibular) containing four samarium cobalt magnets per arch (two on either side) which the author describes as an ‘energized bite block’ ([Figure 13]). The magnets produce a reciprocal repelling, intrusive force of 600*650g per side. [24]

Extractions for open bite closure:
Different types of extractions have been suggested to correct anterior open bite22, including extracting the second molars, extracting the first molars, extracting the second premolars, and extracting the first premolars (Nanda, 2012).
Second molar extractions: The extraction of second molars has been suggested as a practical option in patients who have an anterior open bite with contact solely on these teeth and divergent occlusal planes (wedge effect).
First molar extraction: Typically, the first molar extracted only if they are compromised by extensive decay. If the second molar have not erupted and if the only contact is between the first molar, extraction of first molar would eliminate the increased vertical height
Premolar extractions: Extraction of second or first premolars are the most commonly considered alternatives for the treatment of anterior open bites associated with crowding and or overjet. In patients who has premolars extracted, extrusion of anterior segment rather than wedge effect aids in closing the open bite.
Temporary anchorage devices (tad):
TAD provides a source anchorage for intrusion of molars to correct the vertical dimension without the need for compliance of patient. A major advantage of molar intrusion with TADs is the favourable skeletal changes that enhance a patient’s dentofacial aesthetics. The suggested magnitude of force for molar intrusion is about 50 to 200 g per tooth. For en mass intrusion of premolars and molars, a force of approximately 200 to 400 g has been suggested. Usual time for intrusion of maxillary molars is 5-7 months for a mean intrusion of 2mm to 4mm. Sugawara et al. reported mean intrusion of 1.7mm and 2.8mm for mandibular first and second molars, respectively, when mini- plates were used. Molar intrusion can be accomplished with different types of TADs. The line of force for molar intrusion determines the number of mini-implants, buccal or palatal placement, direct anchorage or indirect anchorage, and anatomic location of TAD placement.
Skeletal anchorage system (SAS)
Mikako umemorl et al., 1999 has described about the skeletal anchorage system for open-bite correction. [25] It consists of titanium miniplate that is temporally implanted in the maxilla (or) in the Mandible as an immobile anchorage. SAS - is used to intrude the Molars to correct the open-bite Malocclusion
Surgical treatment
Hulliten in 1849 was the first to surgically correct an anterior open bite. Since that time the operation was been termed as anterior mandibular sub-apical osteotomy and Trauner, Hofer, and Kole have modified it.
Anterior maxillary and mandibular sub apical osteotomy
A small open bite associated with the minimal tooth exposure (or) none, lip competence, a good nasolabial angle, and adequate lower anterior facial height
If the relationship between the upper lip and concealed maxillary incisors at rest, speech and smiling produces an unaesthetic edentulous appearance.
“Kole” modification of mandibular sub-apical osteotomy
The main objective of this surgery is to c1ose the open-bite by elevating the lower anterior segment and reducing the chin height which includes horizontal sub-apical bone incision and vertical ostectomies in the premolar (or) molar extraction sites. The choice of extraction site depends on the magnitude of the anterior open bite and location of the reverse curve in the mandibular occlusal plane.
The other surgical procedures used for the correction of anterior open bites associated with mandibular prognathism and severe reverse curve with mandibular arch are
Mandibular Body 'step' ostectomy
Mandibular body 'V “ostectomy
Mandibular body 'Y' ostectomy.
Adjunctive surgical procedures
Stability a nd Retention
Cessation of habits and removal of respiratory obstruction might decrease the rate and severity of relapse. Myofunctional therapy and placement of a tongue crib may improve stability in patients, especially with an anterior tongue posture (Miller AJODO 2020). Janson et al. in his study concluded that the long-term stability of corrected open-bite was higher in patient treated with extraction as compared to those who did not have extraction.
Long term studies indicated that orthognathic surgery is an effective method for the management of anterior open-bite. Superior re-positioning of maxilla by one piece Le fort 1 osteotomy is considered one of the most stable procedure in hierarchy of stability. According to a meta-analysis (Greenlee, 2011), correction of open-bite by a surgery is prone to some amount of relapse, although the long-term stability was greater than 75%, possible reason for post-operative relapse is pre-operative orthodontic treatment, type of surgery, type of surgical fixation, condylar positioning during bimaxillary surgery, growth after surgery, and the soft tissue adaptation. Positioners are routinely suggested during retention phase. The elasticity of positioners between the molars applies an intrusive force through daily chewing exercise. Myofunctional therapy and placement of a tongue crib may improve stability in patients, especially with an anterior tongue posture. According to Nanda, masticatory muscle exercise involving a chewing gum or soft bite during retention might add in retaining the obtained result.
Summary
Open bite has a multifactorial aetiology. It is important to consider the growth status of the patient and to differentiate between a dentoalveolar and skeletal open bite. Treatment’s strategies generally focus on the vertical control and/or extrusion of the anterior segments in the growing patient. With the introduction of TAD, skeletofacial changes can also be obtained with molar intrusion in non-growing patients. In patients with severe long face morphology, if aesthetic is the main concern of treatment, then surgical alternatives should be taken into consideration. Although all these treatments provide the possibility of attaining satisfactory outcomes, long term stability remains the major challenge for the orthodontist.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Source of Funding
None.
References
- J H Parker. The interception of the open bite in the early growth period. Angle Orthod 1971. [Google Scholar]
- H D Subtelny, M Sakuda. Open bite: diagnosis and treatment. Am J Orthod 1964. [Google Scholar]
- W R Proffit. Contemporary Orthodontics. 3rd Edn. 2000. [Google Scholar]
- J P Zuroff, S H Chen, P A Shapiro, R M Little, D R Joondeph, G J Huang. Orthodontic treatment of anterior openbite malocclusion: stability 10 years postretention. Am J Orthod Dentofacial Orthop 2010. [Google Scholar]
- C S Ng, W K Wong, U Hagg. Orthodontic treatment of anterior open bite. Int J Paediatric Dent 2008. [Google Scholar] [Crossref]
- . Open-bite Frank W. Worms, D.D.S., M.S.D., Lawrence H. Meskin, and Robert J. Isaacson, AJODO June 1971. . [Google Scholar]
- W R Proffit, H W Fields, D M Sarver. The etiology of orthodontic problems. Contemporary Orthodontic. 3rd Edn.. 2000. [Google Scholar]
- V Sassouni. A classification of skeletal facial types. Amer J Orthod 1969. [Google Scholar] [Crossref]
- T Rakosi, R E Moyers, I Jonas. Orthodontic Diagnosis (Color Atlas of Dental Medicine). 1st Edn.. 1993. [Google Scholar]
- L Davidson. Thumb and finger sucking. Pediatr Rev 2008. [Google Scholar] [Crossref]
- J S Brauer, T V Holt. Tongue thrust classification. Angle Orthod 1965. [Google Scholar] [Crossref]
- W R Proffit. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod 1978. [Google Scholar]
- D J Dung, R J Smith. Cephalometric and clinical diagnoses of open bite tendency. Am J Orthod Dentofac Orthop 1988. [Google Scholar] [Crossref]
- V Sassouni. A roentgenographic cephalometric analysis of cephalo-facio-dental relationships. Am J Orthod 1955. [Google Scholar]
- J R Isaacson, R J Isaacson, T M Speidel, F W Worms. Extreme variation in vertical facial growth and associated variation in skeletal and dental relations. Angle Orthod 1971. [Google Scholar]
- A M Parker, B Fischhoff. Decision-making competence: External validation through an individual-differences approach. J Behav Decision Making 2005. [Google Scholar]
- S Linder-Aronson. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl 1970. [Google Scholar]
- A K Ritto, P Leitao. The lingual pearl. J Clin Orthod: JCO 1998. [Google Scholar]
- J L Spolyar. A Physiologically Designed Habit Appliance. J Clin Orthod: JCO 1974. [Google Scholar]
- A Stellzig, G Steegmayer-Gilde, E K Basdra. Elastic activator for treatment of open bite. Br J Orthod 2014. [Google Scholar] [Crossref]
- M B Stuani, A S Stuani, A S Stuani. Modified Thurow appliance: a clinical alternative for correcting skeletal open bite. Am J Orthod Dentofacial Orthop 2005. [Google Scholar] [Crossref]
- F A Uribe, N Janakiraman, R Nanda. Management of Open Bite Malocclusion. 2015. [Google Scholar] [Crossref]
- Y H Kim. Anterior openbite and its treatment with multiloop edgewise archwire. Angle Orthod 1987. [Google Scholar]
- E L Dellinger. A clinical assessment of the active vertical corrector-a nonsurgical alternative for skeletal open bite treatment. Am J Orthod 1986. [Google Scholar]
- M Umemori, J Sugawara, H Mitani, H Nagasaka, H Kawamura. Skeletal anchorage system for open-bite correction. Am J Orthod Dentofac Orthop 1999. [Google Scholar]
