Introduction
The Temporomandibular joint starts to develop at the 10th week of intrauterine life. It is a ginglymoarthoidal joint that is pivotal for executing the normal functions such as mastication, speech, esthetics, and overall well-being.1
It has certain unique features:
The articulating surfaces are covered not by hyaline cartilage, but by fibroelastic tissue.
The condylar cartilage is considered as a growth center that significantly contributes to the overall growth of the mandible.
It is the only joint in the body that functions bilaterally.
It has an intact disc that is movable during all joint movements and functions as a shock absorber. 1
Over the years the role of occlusion in temporomandibular disorders (TMD) has been extensively debated, leading to many opinions and much controversy. 2 The changes in the joint caused in response to orthodontic therapy as well the adverse reactions caused have been studied. Lack of communication and coordination of research efforts often begins with differences in terminology. In an attempt to coordinate efforts, therefore, the American Dental Association adopted the term temporomandibular disorders, or TM disorders. 3 Temporomandibular joint disorders (TMDs) are defined as the presence of pain, limited mouth opening, or an audible sound heard on joint movement. 4 According to the American Academy of Orofacial Pain, TMD is defined as a group of disorders involving the masticatory muscles, the temporomandibular joint (TMJ) and associated structures. 5
Orthodontics now seeks treat a functional and esthetic occlusal endpoint and at the same time, strives to restore and maintain the normal seated position of the condyles-Centric relation-a mandibular position that produces the greatest neuromuscular efficiency during function from an electromyographic standpoint. The present review was undertaken to facilitate this goal.
Anatomy of the Joint
The temporomandibular joint is an atypical synovial joint of the condylar variety. The components are: Articular eminence, glenoid fossa, condyle, disc, disc ligaments, and synovial membrane, capsule, extracapsular ligaments.6
The condylar covering is sometimes called as fibrocartilage. The condyle is roughly ovoid in shape. It is approximately measuring about 15-20 mm mediolaterally and 8-10 mm anteroposteriorly.
The disc fills the space between the condyle and the temporal bone.It is biconcave in shape. It consists of three parts - anterior band, intermediate zone, and posterior band. It is described as avascular non-innervated fibrocartilage.
The volume of synovial fluid in the superior joint compartment is 1.2 ml, whereas the inferior joint compartment contains 0.9 ml. The fluid exists under negative intra-articular pressure. The surface tension of the synovial fluid allows the spread of fluid over the articular surfaces as a capillary film that permits the lubrication of the joint during condylar movements. It contains a glycoprotein known as lubricin, which serves to lubricate and minimize friction between articular surfaces of synovial joints.6, 7
Functional anatomy of TMJ-Ball on the hill Concept
As proposed by Charles Greene (2018), 8 the mandibular condyle and the glenoid fossa are ‘anatomic neighbours, that do not contact during jaw movements, rather the condyle exhibits a functional relationship with the articular eminence that it slides over during mandibular movements.
In 75% of the normal population the range of motion of the joint extends beyond the articular eminence. During the opening of the jaw, the fibrocartilage covering the condyle extends along the posterior slope of the eminence, past it to the anterior slope. It is not functionally related to the glenoid fossa when the mouth is closed, but instead is resting at a high zone on the hill.
As an individual ages, the elements of the masticatory system age. Teeth wear occlusally, muscles undergo structural change in response to functional demands and the TMJ also changes as a consequence.
How the Condylar Growth Center is Affected
A number of mechanisms have been proposed to explain the modifications occurring in the condylar head under the influence of external forces. The earliest theory was Brodie’s genetic theory that proposed that like the epiphysis of a long bone the mandible also grows downward and forward according to a predetermined genetic sequence. 9
The Lateral Pterygoid Hyperactivity Hypothesis proposed by Chatelier et al,10 by Petrovic and later by McNamara 11 was negated as it proposed that the Lateral Pterygoid muscle attaches to the condylar head or the articular disk, but anatomic evidence to support this was not found. Studies also concluded that LPM traction did not have a pronounced effect on condylar growth.
The Functional Matrix Theory postulated that the principle control of bone growth lies with the soft tissues associated with it. Since there was little explanation of the exact mechanism stimulating condylar growth the validity of this theory was questioned.
Enlow and Hans presented an overall perspective of the mandibular growth occurring as a composite of regional forces and functional agents of growth control that interact in response to specific extra condylar activating signals. These extrinsic signals laid the foundation of the Growth Relativity Hypothesis, which is currently the most accepted hypothesis.
Growth Relativity Hypothesis9
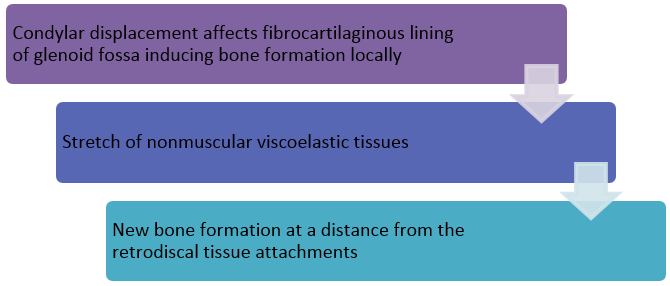
Rather than a factor at work controlling the Condyle-Glenoid fossa modification, a balance of factors is at work when Orthopaedic appliances are used. These include skeletal (displacement), dental, neuromuscular, non-muscular viscoelastic forces including synovial fluids, biodynamic intrinsic and extrinsic factors and maturational age.(Figure 1)
The glenoid fossa and the displaced condyle are both influenced by the articular disk, the fibrous capsule and the synovium, that are contiguous anatomically and functionally, with the viscoelastic tissue.
The synovial fluid dynamics are altered by Orthopaedics. Low intra-articular fluid pressures caused the synovial fluid to shift in a posterior displaced direction. The negative pressures, initially below capillary perfusion pressures, permit the greater flow of blood into the Condyle-Glenoid fossa region.
In accordance with Wolff’s law this hypothesis states that bone architecture is influenced by the neuromusculature and the contiguous, nonmuscular, viscoelastic tissues anchored to the glenoid fossa and the altered fluid dynamics of the enveloping bones.
Light bulb analogy of condylar growth and retention
When the growing condyle is continuously advanced, it lights up like a light bulb on a dimmer switch. When the condyle is released from the anterior displacement, the reactivated muscle activity dims the light bulb and returns it close to normal growth activity. In the boxed area, the upper open coil shows the potential of the anterior digastric muscle and other peri-mandibular connective tissues to reactivate and return the condyle back into the fossa once the advancement is released. The lower coil in the box represents the shortened inferior LPM. The open coil above the yellow condylar light bulb represents the effects of the stretched retrodiskal tissues.
Growth restriction
In normal individuals the glenoid fossa grows in a posteroinferior direction .The articular eminence undergoes extensive resorption at its anterior slope in the posteroinferior direction and the posterior slope undergoes compensatory endosteal deposition up till 7 years of age.Posteriorly directed forces of the viscoelastic forces ,cause the fossa to relocate anteroinferiorly to meet the active condylar modification and restore normal function during Orthopaedic treatment, thus contributing towards class II correction. This growth restriction combined with maxillary growth restriction, results in the mandible growing downward and forward.
Retention relapse of condylar modification
Active return of the condyles to the fossae post-treatment deactivates the modifications by compressing the condyle against the proliferated retrodiskal tissues. Any additional bone induction appears to be clinically insignificant in the long term. Condylar cartilage is the mechanical supporter that mends and extends itself in an attempt to regain function in the displaced condition when it is affected by environmental and functional factors including the function of the condyle within the Glenoid fossa.
Effect Observed during Orthodontic Treatment
Functional and Orthopaedic appliances affect anteroposterior and vertical changes by differential eruption of the dentition, as well as Condylar displacement and viscoelastic tissue forces. The response seen by appliances was-
Twin block
This was designed by Dr.William Clark in 1977. Twin Block appliance was designed for full time wear, including during eating. An edge-to-edge bite with a small inter-incisal space, typically 2 mm, encourages the patient to close the lips naturally. This posture is reinforced as the patient eats and drinks with the appliances in the mouth. Twin Block appliance therapy increases dimensions of mandibular condyle in the three planes of space and reposition toward a more forward position.
Increased posterior and superior and decreased anterior and medial joint spaces are another indication of anterior and inferior positioning of the condyle.
As a result the mandible postures downward and forward.
Significant improvement of the skeletal profile in anteroposterior and vertical direction; most of these changes were due to an increase in the effective mandibular, ramus,and corpus lengths and increase in posterior facial height, respectively. 12, 13, 14
Frankel regulator
The Temporomandibular joints in patients undergoing treatment using the Frankel (FR-II) appliance, used for the correction of Class II malocclusion when observed using MRI exhibited configuration changes in the shape of the articular disk at the end of the treatment.
The disc was considered biconcave (normal) if the anterior and posterior band expansions were anterior and above the condyle in parasagittal views and arc-shaped over the condyle in the closed-mouth coronal plane. Any enlargement, folding, or deformation of the bands of the disc (biconvex or biplanar) not related to normal anatomic variations in disc size and thickness was classified as a non-biconcave shape. No positional changes occurred in the discs. 15, 16
Regarding the change in the position of the mandibular condyle to the crest of the eminence at the beginning of treatment and after functional appliance therapy, the study conducted by Gianelly et al. concluded that condyles were repositioned inferiorly in centric occlusion after 1 year of therapy. 15, 16, 17
Bionator
The appliance was developed by Balters in 1950s.It differed from a conventional activator in that it was less bulky and more elastic. Studies conducted by A.M Arujio et al.(2004) 18 compared the differences in condylar growth between control groups and those that received bionator therapy and concluded that posterior growth changes were greatest in the condylar region for the bionator group, however these changes were not statistically significant.
In a study conducted by Chavan et al.(2014), 19 he concluded that following treatment with the appliance the condyles occupied a more anterior position in the fossa to its pre-treatment position, while the disk moved more posteriorly in relation to the condyle. Although the treatment group showed consistent forward positioning of the condyle and backward movement of the disk, long-term MRI findings in these groups will further clarify the adaptations between the condyle fossa and articular disk.
Protraction facemask 20, 21
PFM usually consists of a forehead support, a metal frame and a chin cup as an anchorage unit. As the chin serves as the anchorage region in this kind of device, a clockwise rotation force is applied directly to the mandible, causing it to be displaced downward and backward during treatment and resulting in an increased mandibular plane angle. Facemask therapy for maxillary protraction in management of skeletal class III produced:
1- Decrease in both posterior and superior joint spaces, while increase in the anterior joint spaces.
2- Bone remodeling in the glenoid fossa causes upward and backward displacement of the condyle.22
Activator
Results showed that the disc is not impaired by Activator therapy; it seems possible that adaptive remodeling, including a shallower glenoid fossa and increased condylar height, was seen after treatment.23 Overall, condylar height showed a significant increase, and the eminence angle decreased. TMJ disc length has no statistically significant change before and after treatment. A slight advancement was found in the sagittal condylar position. A significant backward movement was shown in the sagittal disc position. Our results showed that the disc is not impaired by Activator therapy; it seems possible that adaptive remodeling, including a shallower glenoid fossa and increased condylar height, was seen after treatment. 24
TAD anchored maxillary protraction-Studies have
Shown an increase in bone deposition at the anterior wall of the TMJ and resorption at the posterior wall when bone anchored TAD maxillary protraction. 25
Temporomandibular Joint Disorders
Craniomandibular disorders is a collective term embracing a number of clinical problems that involve the masticatory musculature,the temporomandibular joint or both.It is synonymous with the term Temporomandibular disorders.
Classification
Classification systems have been based on signs and symptoms, tissues of origin, etiology, structural and functional disorders, frequency and medical classification. From a clinical perspective they can be divided into-
Treatment Modalities
These modalities have been divided into four groups:
Baseline records- A well-organized, disciplined approach to fact finding should be used to develop the necessary baseline records to provide a viable diagnosis and plan of treatment. The necessary baseline records should include a comprehensive history, a thorough clinical examination, radiographic surveys, diagnostic casts and other indicated diagnostic tests or consultations. The baseline records are listed and all are clinically and/or scientifically documented.
Behavior modification- Modalities that come under the classification of behavior modification are considered when the clinical impression is that the psychophysiological or nonorganic aspects of the patient’s symptoms outweigh the clearly physical or organic aspects. Usually the symptoms are nonarticular or periarticular as to location rather than articular.
Repair and regeneration-Treatment modalities that assist in repair and regeneration of the tissues of the masticatory system are considered when the physical or organic aspects of the patient’s symptoms dominate the psychologic or nonorganic aspects.
Orthopedic stabilization- Definitive treatment of the masticatory system should be deferred until after the acute symptoms have been controlled and a subsequent evaluation made. Muscle splinting or edema within the joint, for example, can cause a transitory malposition of the condyle within the fossa, resulting in a gross malrelation of opposing teeth.
It is not always necessary to alter the occlusion after the acute condition has been controlled, providing the occlusal relationships return to an acceptable state.
Conclusion
The temporomandibular joint is one of the most complicated working assemblies in the human body. No orthodontic procedure can be performed in isolation without considering its possible effect on the temporomandibular joint When planning a treatment for patients afflicted with this disease considerations should be made to alleviate the problem.
Etiologic factors that might cause upward and backward pressures on the mandible should be reduced as much as possible.
Mechano therapy that may cause upward and backward pressures on the condyles are not recommended. Final detailed correction of dental abnormalities should always consider optimal temporomandibular health and function.
Retention procedures should be planned to provide a proper path of closure to minimize or prevent possible retrogressive post-treatment changes.
Appliance therapy used in orthodontics works to harness the inherent growth potential of the jaws in growing patients, often of the temporomandibular joint cartilage, that can result in the growth of the mandible. Thus the temporomandibular joint essential for the orthodontist. We must not add to TMJ disorders by mistreatment and confirm the “law of unintended consequences”.