- Visibility 54 Views
- Downloads 3 Downloads
- DOI 10.18231/j.ijodr.2021.021
-
CrossMark
- Citation
Facial asymmetry: A review
- Author Details:
-
Ankit Mishra *
-
Ragni Tandon
-
Aftab Azam
-
Kamlesh Singh
-
Pratik Chandra
-
Shreya V Mishra
Introduction
The terminology "asymmetry" refers to variance among homologous parts that affects structural balance. Face and dentition asymmetry might occur spontaneously or as a result of trauma. Facial asymmetry is often indicated by studying the homologous region of the face. The assessment of facial asymmetry includes a patient interview with the orthodontist, extra-oral and intra-oral clinical examinations, and supplemental examinations. Treatment options range from asymmetrical orthodontic mechanics to orthodontic surgery, depending on the patient's age, the primary aetiology of the disease, and the degree of incompatibility.[1] The symmetry of the components of the right and left sides of the face is crucial to study, as some degree of facial asymmetry is observed in virtually everyone and is regarded normal because the right and left sides of the face are not exact carbon copies of each other.
Many human body components develop bilaterally symmetrically. As a result, the right and left sides can be separated into mirror images. A minor degree of symmetry is common in the face. Nonetheless, mild asymmetry, also described as relative asymmetry, subclinical asymmetry, or normal asymmetry, goes unnoticed by the carrier and those around them.[1] However, whenever the degree of asymmetry is significant, the problem is usually visible, which has a detrimental impact on one's facial and grin aesthetics.
When related to facial morphology, harmony and balance apply to the state of face equilibrium: the correspondence in size, shape, and organization of facial features on opposite ends of the median sagittal plane. Because many faces appear harmonious and well proportioned on clinical soft tissue evaluation, cephalometric X-ray examinations have shown that all faces exhibit various degrees of craniofacial asymmetry.[2]
Absolute bilateral bodily symmetry is a theoretical idea that is rarely found in living beings. Right-left differences can be seen anywhere in nature when two congruent but mirror image kinds coexist. People commonly exhibits functional and morphological asymmetries, such as right and left handedness, as well as a predilection for one eye or one leg. Some of these asymmetries have embryonic roots and are connected with central nervous system asymmetry.[3]
Facial asymmetry being a common phenomenon, was probably first observed by the artists of early Greek statuary who recorded what they found in nature-normal facial asymmetry. When the amount of asymmetry is significant, the problem is usually visible, which has a detrimental impact on one's facial and smile aesthetics. Facial asymmetry in the craniofacial complex ranges from barely discernible to obvious differences between the right and left half of the face.[4]
Dental malformations have been linked to taunting and general playground harassment in youngsters, as well as a decrease in social attractiveness. Facial appearance is a crucial variable in the development of first impressions, and there is ample evidence that unattractive persons are seen as less socially adept, less popular, and less pleasant in the absence of additional information. In two separate trials, patients undergoing orthognathic surgery were questioned prior to surgery. Over 60% of patients said their facial appearance had a negative impact on their personal life, and 40% said it had a negative impact on their social life.[4]
Background and Significance of Facial Asymmetry
Artists such as Leonardo da Vinci and Albrecht Dürer believed that the human body and face expressed symmetry and used this philosophy in their art work. However, in 1887 the Greek artist, Hasse, noted that asymmetry of the craniofacial complex was a common occurrence and sculptors at that time reproduced this in their art. The debate on symmetry was not confined to the world of art. A German orthodontist, Simon (1924), stated “bilateral symmetry is a most manifest morphological characteristic of the body and especially the head.” However, further investigations into symmetry dispel this notion, therefore agreeing that a certain unquantified level of asymmetry can and should be accepted as normal. However, skeletal asymmetry may be completely or partially masked by the soft tissues (Haraguchi et al, 2002).[5] Despite the potential camouflage provided by the soft tissues investigators found that asymmetry is also a common occurrence in the facial soft tissues.
Farkas and Cheung (1981) examined over 300 subjects in three age groups (6, 12 and 18 year olds) for facial asymmetry using direct anthropometry. Their measurements included point to point distance and angular measurements and they found average differences between the right and left sides were mild in both the absolute measurements (3mm) and relative values (3%).[6]
Etiology of Facial Asymmetry
According to Cheong and Lo reported that the causes of facial asymmetry can be grouped into three main categories 1) congenital, of prenatal origin, 2) accquired, resulting from injury or disease and 3) developmental, arising during development and of unknown etiology ([Table 1])[7]
|
Congenital factors |
Acquired factors |
Developmental factors |
|
Cleft lip or palate |
Temporomandibular joint ankylosis |
Unknown etiology |
|
Hemifacial Macrosomia |
Facial trauma |
|
|
Neurofibromatosis |
Children’s radiotherapy |
|
|
Conginital muscular torticollis |
Fibrous dysplasia |
|
|
Craniosynostosis |
Facial tumors |
|
|
Vascular disorders |
Unilateral condylar hyperplasis |
|
|
|
Parry-romberg syndrome |
|
Classification of Facial Asymmetry
The asymmetries were classified as dental, skeletal, muscular and functional by Bishara et al.[8] Similarly Obwegeser and Makek[9] classified asymmetries as hemimandibular elongation or hemimandibular hyperplasia. When there is an increase of the condyle or the ramus in the vertical plane or an increase of the mandibular body in horizontal plane. While in hemimandibular hyperplasia there is an increase on one side of the mandible as a whole. Hwang [10] established four types of asymmetry depending upon the skeletal analysis of deviation of the chin and bilateral difference between mandibular rami length. The four types are patient with deviation of the chin and bilateral difference between the mandibular rami length; patient with bilateral difference between mandibular rami length, only; patient with deviation of the chin, only; and patients with change in volume on one side of the mandible, only, without deviation of the chin or discrepancy between mandibular rami length.
Facial asymmetry by TML system
This system purposes to classify facial asymmetry with accompanying mandibular prognathism to facilitate choice of surgical methods. 153 of the patients were diagnosed with facial asymmetry based on menton deviation criteria assessed through PA cephalograph and transverse asymmetry evaluated using an actual size (1x1) clinical photo. The exclusion criteria used were: (1) previous orthognathic surgery, (2) an existing medical, physical or mental condition that would impair healing potential, (3) syndromic craniofacial deformities and (4) pathologic conditions such as condylar elongation, unilateral condylar hyperplasia and hemimandibular hypertrophy. The diagnosed patients consisted of 86 males and 67 females with an age range from 15 to 46 and a mean age of 22.3 years. Clinical photographs were taken in an audio-visual room and printed at actual size by measuring the length from the end of the right eyebrow to the chin. Additional clinical photographs taken in the department were also printed at actual size by measuring the length of the inner canthus. PA cephalometry was recorded using a Cranex 3þ Cep (Soredex, Finland) on 1000 _ 1200 X-ray film with an exposure of 10 Ma, 77 Kvp for 0.8 s. The radiographs were traced on 0.12 mm tracing paper with a 0.3 mm black pencil. Reference points up to 0.5 mm were measured on tracing paper. Average values were obtained after measurements by a single individual. [11]
Measurement in actual sized (1x1) clinical photos
Reference point – External canthus (EC), upper stomion (Ustm), soft tissue gonion (SG), soft tissue mandibular midline point (SMm), lip commissure (LC), and midpoint of pupil (Pm) were set as reference points.
Reference lines – lines were drawn connecting each external canthus and lip commissure, designated as horizontal reference line (HRL) and lip line (LL) respectively. The soft tissue midsagittal line (STML) was set as the line perpendicular to the HRL, passing through the centre of both Pm and the ridge of the nose as shown in [Figure 1].
Measurement – the distance from SMm to STML (DSm), SG to STML (DSG) and LL to Pm (DPm) were measured. The direction was ignored.
Analysis – asymmetry was diagnosed when (DSm) was more than 2.0 mm and defined as soft tissue menton deviation. Lip canting was defined as difference in vertical growth (DPm) exceeding 2.0 mm. Transverse soft tissue asymmetry was defined as DSG greater than 2.0 mm.
Radiographic measurements
Reference points – Molar point (M), menton point (Mm), gonion (G), latero-orbitale (Lo), crista galli (CG), and anterior nasal spine (ANS) were set as reference points.
Reference line – the line connecting ANS and CG was drawn as the midsagittal line (MSL). The line perpendicular to the MSL passing through Lo, located below, served as the horizontal reference line (Z-line) as shown in [Figure 2].
Measurement – the distances from Lo to M point (DloM), MSL to Mm (Dm) and MSL to G (DG) were measured. The direction was ignored.
Analysis – Asymmetry was diagnosed when Dm exceeded 2.0 mm and defined as menton deviation. Maxillary canting was defined as difference in vertical growth (DloM) exceeding 2.0 mm. Transverse hard tissue asymmetry was defined as (DG) greater than 2.0 mm.
Classification of Facial Asymmetry according to the combination of menton deviation and transverse asymmetry (T-group)
T1: Equal direction of menton deviation and transverse soft tissue asymmetry.[Figure 3].
Subclassification of transverse asymmetry according to direction of angle prominence in soft vs hard tissue.
H1: Equal direction of transverse asymmetry in soft vs hard tissue.[Figure 4].
Classification of asymmetry based on the combination of deviation of menton and cant in soft and hard tissue.
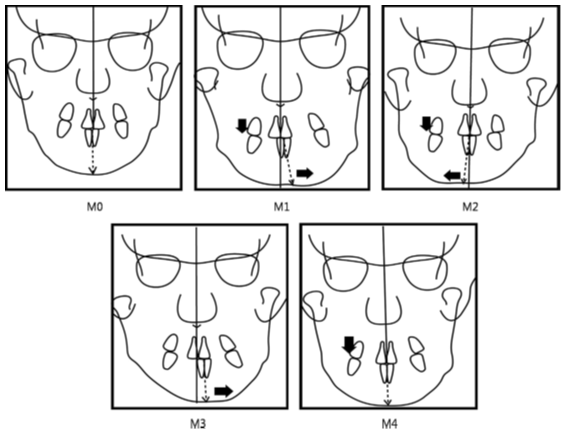
Classification in hard tissue
M0: Neither maxillary cant nor menton deviation.
Classification in Soft tissue
L0: Neither lip canting nor soft tissue menton deviation.[Figure 6]. [11]
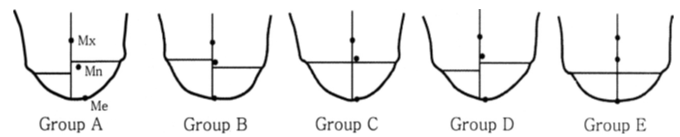
Classification of facial asymmetry by cluster analysis
Mild facial asymmetry was regarded by clinician because it was believed that normal craniofacial skeleton had some asymmetry, and that this was subclinical and could be compatible with normal dental occlusion.
The purposes of this study were to classify patients with facial asymmetry by using the cluster analysis technique on the basic of the craniofacial measurements related to asymmetry and to evaluate the characteristic of the resultant groups according to the measurements.[12]
Menton (Me) deviation (X1): angle formed by the crista galli – Me line and MSR.
Apical base midline discrepancy (X2): horizontal distance between the midpoints of the maxillary central incisor roots and the mandibular central incisor roots.
Vertical difference of right and left antegonion (X3): vertical distance between right antegonion (Ag) and left Ag.
Horizontal difference of right and left Ag (X4): difference between horizontal positions of the right Ag and left Ag.
Maxillary base canting (X5): angle formed by the line connecting the right and left jugal points and the horizontal reference line, which is vertical to MSR.
Maxillary alveolar canting (X6): angle formed by the line connecting the right and left points constructed with the buccal contour of the first molar and the adjacent alveolar bone contour and the horizontal reference line.
Bulkiness difference of mandibular inferior border (X7): difference between the right and left bulkiness of the mandible determined subjectively as a number from 1 to 5, with a larger number for more severe asymmetry.
Lip line canting (X8): angle formed by the line connecting the right and left commissures of the lip and the interpupillary line as shown in [Figure 7].
The cluster analysis technique divided the 100 patients into 5 groups with different characteristic as shown in figure 8.
Group A showed a distinct difference of right and left ramus length. Me was deviated to the side of the shorter ramus. Mandibular apical base midline also was deviated to the same side. Lip line canting also is distinct in this type of asymmetry. Group A has a typical type of asymmetry; its etiology is believed to be asymmetric condylar or whole mandibular growth. With asymmetric mandibular growth, the chin deviates to the side of the shorter ramus. Compensatory asymmetric vertical growth of the maxilla is common in this type of asymmetry, contributing to cants of the maxilla and the lip line.
Group B showed the same ramus length difference between the right and left sides as group A, but Me deviation was different. Me was deviated in the opposite direction to shorter ramus, indicating that the etiology of group B was not related to asymmetric condylar growth. Waugh, 15 in a study on the influence of diet on the jaws and faces of American Eskimos, indicated that the difference of chewing force affects the form of the jaws and the face. Tay16 suggested that unilateral mastication has a certain association with mandibular asymmetry. Ingervall, in an electromyographic study to investigate the correlation between muscular activity and facial morphology, showed that subjects with marked activity in the masticatory muscles had shorter face height—the so-called “low angle.” Considering all these studies, it is likely that the asymmetry in group B resulted from unilateral mastication: the chewing side of the jaw develops a low angle, and the non-chewing side develops a high angle. In addition to different angle shapes between the right and left sides, soft-tissue asymmetry can result from unilateral muscle hypertrophy on the chewing side. Various causative factors such as missing teeth, scissors-bite, occlusal interference, and faulty restorations on 1 side might be responsible for this type of asymmetry.
Group C had a specific characteristic: no ramus length difference between the right and left sides but Me and lower apical base midline deviations to 1 side. The reason for this asymmetry is a functional shift of the mandible that results from various types of occlusal interference such as a malposed tooth, a crossbite of at least 1 tooth, or a constricted maxillary arch. Abnormal tooth contact causes the subsequent mandibular displacement in maximum intercuspation. Schmid et al described this type as displacement asymmetry; other asymmetries were structural. Joondeph, in a recent review, called this type functional asymmetry and suggested intercepting it at an early stage because the condyle and the fossa adapt easily to the deviated mandibular position.
Group D were similar to group A. The only difference was in magnitude. A separate cluster was formed in the analysis because all variables showed small discrepancies. Although the treatment modality for this group would be the same as for group A, camouflage treatment could be a good option without correction of face, because the degree of asymmetry is not great.
Group E showed minimal values in all variables, indicating that these subjects were within normal limits. Relatively many subjects, 28%, were included in this cluster, because our subjects were patients who had frontal cephalograms taken for diagnosis, regardless of existence or severity of facial asymmetry. [12]
Diagnostic Methods
The evaluation of the asymmetric patient necessitates distinguishing between oral and skeletal abnormalities. Although the clinical examination provides a wealth of information, cephalometric analysis and study models provide critical hints in the diagnosis of skeletal disparity.
The first step in the diagnosis of all patients is to identify these asymmetries and to differentiate between those that have a dental or a skeletal cause. It is only then that the clinician can make a valid decision concerning the need for surgery or a non-surgical approach and, if the approach is non-surgical, if extraction or non-extraction is the treatment of choice. The diagnosis of skeletal or dental asymmetry can be accomplished by an overall evaluation of the patient’s skeletal or soft-tissue facial pattern. Radiographs, such as postero-anterior and submental views, are particularly useful in making this type of diagnosis. The submental vertex is particularly useful in the diagnosis of mandibular asymmetry. Specialised radiographs, such as computed tomographic scans and the use of stereometry with or without implants, offer much information but are demanding for average patients. The soft tissues of face also offer a clue to any existing skeletal problem. Close observation during the clinical examination, both from frontal and inferior aspect, along with oriented facial photographs is a necessary requirement for proper diagnosis.[13]
In order to assess asymmetry, patient must be in upright position, looking forward with teeth in normal occlusion and relaxed lips. A common procedure which could be implemented by the use of dental floss stretched from the region of the glabella to the lower chin, passing through the philtrum. In order to assess the ooclusal plane in vertical direction patient is asked to bite a wooden sheet which is correlated with the pupillary plane on both sides. As per Padwa et al, [14] an inclination of the occlusal plane greater than four degrees causes significant asymmetry on the person’s face. Clinical diagnosis should be supplemented with various diagnostic procedures such as dental casts, photographs, radiography, tomography, and bone scintigraphy in order to appropriately find and evaluate the structures involved in asymmetry.
At present the assessment of craniofacial asymmetries is done using the computed tomography especially cone-bean computed tomography (CBCT). [15] A CBCT scan of the head usually produce a effective radiation dose that is lower than that of all supplementary radiographic examinations required for complete orthodontic records taken for asymmetry assessment purposes and further provided a detailed diagnosis. [16] Various asymmetries are shown in [Figure 9] which provide us with information about the effectiveness of CBCT in detailed examination of the structures. [17]
Treatment of Asymmetries
The orthodontic corrections of dental asymmetries are often considered a difficult and challenging process, primarily because of misdiagnosis and poorly planned treatment mechanics. A careful differential diagnosis together with a through treatment plan can ensure successful treatment outcomes in the management of these malocclusions. Early detection of the asymmetric malocclusion, as well as correct diagnosis and treatment planning, are essential for optimal treatment outcomes. The orthodontic therapy of a malocclusion with any degree of asymmetry is typically difficult because asymmetric mechanics in the right and left quadrants of the dental arch are required to accomplish adequate correction.
Bishara et al [3] suggested that asymmetry must be differentially diagnosed as being either the result of skeletal asymmetry, asymmetry within the dental arches, discrepancies between centric occlusion and centric relation or a combination.
Treatment of dental asymmetries
Treatment of dental asymmetries - true dental asymmetries such as, with a congenitally missing lateral incisor or second premolar, is often treated orthodontically. Asymmetric extraction sequences and asymmetric mechanics. E.g. Class III elastics on one side and Class II elastics on the other with oblique elastics anteriorly, can be used to correct, dental arch asymmetries. Composite build-ups or prosthetic restoration may be indicated with pronounced tooth irregularities.
Treatments of functional asymmetries
Treatments of functional asymmetries – mild deviations due to functional shifts are often corrected with minor occlusal adjustments.Orthodontic therapy is required for more severe aberrations in order to align the teeth and restore appropriate function. Occlusal splints may be required to accurately assess the existence and amount of the functional change by removing habitual postures and deprogramming the muscles. Because functional shifts can be caused by skeletal asymmetry, fast maxillary expansion, orthognathic surgery, and orthodontic treatment may be indicated in the treatment of these issues.
Treatment of skeletal asymmetries
Treatment of skeletal asymmetries- the severity and nature of the skeletal asymmetry whether the discrepancy can be completely or partially resolved through orthodontic treatment. In growing patient, orthopaedic appliances in conjunction with orthodontic treatment are used to help improve or correct the developing asymmetries. [18]
Aymmetries of skeletal nature treated with orthodontics alone might dictate certain compromises that need to be explained to the patient before treatment is initiated. Severe misalignments may necessitate a mix of surgery and orthodontic therapy. A thorough examination will aid in determining whether the maxilla and/or mandible will require surgical relocation.
Abnormalities in the coronoid and condylar processes as well as in position and shape of the articular disc should be considered whenever limited opening, acute malocclusions or mandibular deviations are found.
Treatment of skeletal asymmetries
Treatment of soft tissue asymmetries- deformities due to soft tissue imbalance can be treated by either augmentation or reduction surgery. Augmentations include the use of bony grafts and implants to recontour the desired areas of the face.
With mild skeletal, dental or soft tissue deviations the advisability of treatment should be carefully considered. [3]
Treatment of Dental Asymmetries
In orthodontics, the dental asymmetries is divided into four groups. 1) diverging occlusal planes. In this for the correction of canted anterior occlusal plane the use of vertical inter-arch elastics given to extrude the side of the occlusal plane that is farthest from the treatment ooclusal plane. For unilateral extrusion of canted anterior segment, 0.017x0.025 inch TMA cantilever can be used coming from auxiliary tube of molar on the side where the extrusion is to take place and is hooked around the anterior segment as shown in [Figure 10]. [19] For the canted posterior occlusal plane (in anteroposterior direction) a variation in intrusion arch can also be used. To upright the buccal segment, a cantilever with hook can be used but it has side effects which are leading to extrusion of buccal segment and unilateral intrusion of anterior segment as shown in [Figure 11]. 2) Asymmetric left or right buccal occlusion. A molar rotation is frequently seen in maxillary arch. A mesial-in rotation of one molar often result in an asymmetric molar occlusion. To correct this a transpalatal arch is used with equal amount of anti-rotation activation as shown in [Figure 12]. 3) Unilateral dental crossbite. For the treatment of unilateral dental crossbite a lingual arch in mandible and transpalatal arch in maxilla can be used. TPA is inserted as such the horizontal part of the TPA will be occlusal to the bracket on the cross bite side. In addition, expansion activation should be built into the transpalatal arch as shown in [Figure 13]. 4) Asymmetric arch form. Orthodontist use asymmetrically shaped archwire or a asymmetric interarch elastics to correct asymmetric arch form. It is important to correct asymmetry in buccal occlusion during the early stages of treatment. This helps the orthodontist to use symmetric mechanics during remainder of treatment.[19]











Surgical Treatment for Asymmetry in Adults
In adults, skeletal asymmetry cannot be managed orthodontically. The general approach is the same as for any other type of surgical-orthodontic treatment: a fixed orthodontic appliance is placed a few months before surgery so that initial alignment of the teeth can be achieved, jaw surgery is done as necessary to correct the asymmetry, and the appliances are used for finishing orthodontics.
For these patients, the major treatment planning decision is the extent to which surgery will be used to correct the deformity at its point of origin, as opposed to compensating for existing deformity and in essence camouflaging it. For example, an asymmetric mandible can be treated by surgery in the ramus, correcting the unequal ramus length that is a major cause of the deformity or it can be managed by inferior border osteotomy to slide the chin sideways, correcting the obvious asymmetry anteriorly and leaving the gonial angles as they were. Similarly, an asymmetric maxilla could be corrected by rotating the entire upper jaw or camourflage by asymmetric onlay graft. [20]
Treatment of hemimandibular hypertrophy (Condylar hypoplasia)
When hemimandibular hypertrophy is first discovered, the key question is whether the deformity is progressive (i.e. whether excessive growth is continuing). If the asymmetric growth stops and the condition are stabilised, it is preferable to delay surgery until the patient is a young adult and to correct the asymmetry without involving the temporomandibular joint. If the asymmetry is already severe enough to cause a problem and is becoming progressively worse, there is no option, even in young patients, but to remove the growth site at the head of the affected condyle. In some patients, the head of the condyle remains approximately normal in size, but the length of the condylar neck increases, in others the condylar head is enlarges.
A 99 mtechnetium phosphate bone scan is the most direct way to determine whether asymmetric growth is still occurring. More uptake of the isotope on the affected side than on the unaffected one indicates active asymmetric growth. Unfortunately although false positives are rare, false negatives occur with this diagnostic approach. Clinical observation of counting growth may indicate surgery to remove the affected condyle even through repeated bone scans do not demonstrate continued isotopes uptakes.
If progressively deformity requires removing the condylar growth site, the surgical options for the affected side are (1) excision of bone at the head of the condyle, then re-contouring or repositioning the bony stump or (2) removing the condyle and condylar process and reconstructing the area either with a costochondral junction transplant as, or with a free graft. In addition, a sagittal-split osteotomy on the unaffected side almost always is needed to allow proper positioning of the mandible. In an adult, if the maxilla is canted because of excessive vertical growth on the affected side, maxillary surgery also required. In younger patients, a hybrid functional appliance can be used post-surgery to improve the maxillary cant by blocking further eruption of teeth on the affected (long) side and allowing teeth to erupt on the unaffected (short) side. Because the body of the mandible bows downward on the affected side, re-countering of the lower border is likely to be needed as a secondary procedure, but maxillary surgery often can be avoided. [21]
Conflict of Interest
The authors declare that there is no conflict of interests
Source of Funding
None.
References
- G Thiesen, BF Gribel, MP Mota Freitas. Facial asymmetry: a current review. Dent Press J Orthod 2015. [Google Scholar] [Crossref]
- S Peck, L Peck, M Kataja. Skeletal asymmetry in esthetically pleasing faces. Angle Orthod 1991. [Google Scholar]
- SE Bishara, PS Bishara, JG Kharouf. Dental and facial asymmetries: a review. Angle Orthod 1994. [Google Scholar]
- C Phillips, ME Bennett, HL Broder. Dentofacial disharmony: Psychological status of patients seeking treatment consultation. Angle Orthod 1998. [Google Scholar]
- S Haraguchi, K Takada, Y Yasuda. Facial asymmetry in subjects with skeletal class III deformity. Angle Orthod 2002. [Google Scholar]
- G Farkas, G Cheung. Facial asymmetry in Healthy North American Caucasians. An Anthropometric study. Angle Orthod 1981. [Google Scholar]
- YW Cheong, LJ Lo. Facial asymmetry etiology, evaluation and management. Chong Gunj Med J 2011. [Google Scholar]
- SE Bishara, PS Buurkey, JG Kharouf. Dental and facial asymmetries a review. Angle Orthod 1994. [Google Scholar]
- HL Obwegeser, MS Makek. Hemimandibular hyperplasia — Hemimandibular elongation. J Maxillofac Surg 1986. [Google Scholar] [Crossref]
- H S Hwang, JA McNamara. A new classification of facial asymmetry. Early orthodontic treatment is the benefit worth the burden? Ann Arbor University of Michigan . [Google Scholar]
- JY Kim, HD Jung, YS Jung, CJ Hwang, HS Park. A simple classification of facial asymmetry by TML system. J Cranio-Maxillofac Surg 2014. [Google Scholar]
- HS Hwang, IS Youn, KH Lee, HJ Lim. Classification of facial asymmetry by cluster analysis. Am J Orthod Dentofac Orthop 2007. [Google Scholar]
- CJ Burstone. Diagnosis and treatment planning ofpatients with asymmetries. Semin Orthod 1998. [Google Scholar] [Crossref]
- BL Padwa, MO Kaiser, LB Kaban. Occlusal cant in the frontal plane as a reflection of facial asymmetry. J Oral Maxillofac Surg 1997. [Google Scholar] [Crossref]
- SJ Yoon, RF Wang, HJ Na, JM Palomo. Normal range of facial asymmetry in spherical coordinates: a CBCT study. Imaging Sci Dent 2013. [Google Scholar]
- DC Lorenzoni, AM Bolognese, DG Garib, FR Guedes, EF Sant’Anna. Cone-Beam Computed Tomography and Radiographs in Dentistry: Aspects Related to Radiation Dose. Int J Dent 2012. [Google Scholar] [Crossref]
- C Baek, JY Paeng, JS Lee, J Hong. Morphologic Evaluation and Classification of Facial Asymmetry Using 3-Dimensional Computed Tomography. J Oral Maxillofac Surg 2012. [Google Scholar] [Crossref]
- KV Sarnäs, H Pancherz, B Rune, G Selvik. Hemifacial microsomia treated with the Herbst appliance. Am J Orthod 1982. [Google Scholar] [Crossref]
- E Steenbergen, R Nanda. Biomechanics of orthodontic correction of dental asymmetries. Am J Orthod Dentofoc Orthofac Orthop 1995. [Google Scholar] [Crossref]
- HL Legan. Surgical correction of patientswith asymmetries. Semin Orthod 1998. [Google Scholar] [Crossref]
- GE Erickson, DE Waite. Mandibular asymmetry. J Am Dent Assoc 1974. [Google Scholar] [Crossref]
- Introduction
- Background and Significance of Facial Asymmetry
- Etiology of Facial Asymmetry
- Classification of Facial Asymmetry
- Facial asymmetry by TML system
- Measurement in actual sized (1x1) clinical photos
- Radiographic measurements
- Classification of Facial Asymmetry according to the combination of menton deviation and transverse asymmetry (T-group)
- Subclassification of transverse asymmetry according to direction of angle prominence in soft vs hard tissue.
- Classification of asymmetry based on the combination of deviation of menton and cant in soft and hard tissue.
- Classification of facial asymmetry by cluster analysis
- Diagnostic Methods
- Treatment of Asymmetries
- Treatment of dental asymmetries
- Treatments of functional asymmetries
- Treatment of skeletal asymmetries
- Treatment of skeletal asymmetries
- Treatment of Dental Asymmetries
- Surgical Treatment for Asymmetry in Adults
- Conflict of Interest
- Source of Funding
