Introduction
Dental caries is still a major public health problem despite the fact that different forms of prophylactics have led to a significant decline in caries rates in the past 50 years.1, 2 The permanent first molar (FPM) is the most caries prone tooth in the permanent dentition.3 FPM also often have some form of hypoplasia with rates ranging from 6% to 10-19% according different studies.3
Deeply decayed first permanent molars in a child are challenging for the pediatric dentist because of the patient’s inability to withstand long treatment under local anesthesia,the degree pulp maturation, and the fact that these teeth often have significant destruction of the crown. Even though adequate treatment results are achieved at the time, these teeth still are likely to have a poor prognosis and require extraction later on. 4
These cases also present a major dilemma to the orthodontist because the first permanent molar has a major role in maintaining normal masticatory function and dentofacial harmony and therefore it is rarely the tooth of choice for extraction for orthodontic treatment. 3, 5 Moreover, children who require extraction of compromised FPM s have poor oral health and are poor candidates for future orthodontic treatment.
That is why the pediatric dentist, and the orthodontist must work as a team and consider many factors before determining the appropriate treatment method for a badly decayed FPM: the long-term prognosis of the endodontic treatment and the restoration;the overall oral health of the patient; the dental age of the patient; the type of malocclusion (Angle's Class I, II, or III); the degree of crowding present; presence and position of third molars; the skeletal pattern of growth.
This is a complex problem, and that is why there is no consensus in the literature for the treatment of children with significantly decayed FPM. Early extraction of first permanent molars have certain consequences in the permanent dentition and the need for the orthodontic treatment must be assessed.6
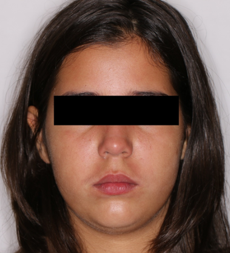
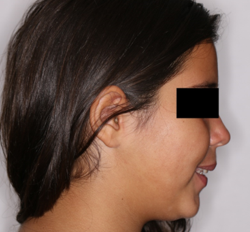
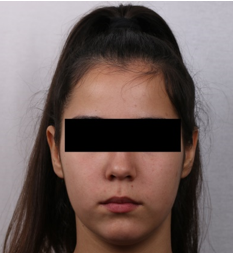
The aim of this clinical report is to present a complex interdisciplinary treatment approach for an 11-year-old girl with history of early childhood caries and multiple restorations on her permanent upper front teeth and all 4 first permanent molars which had apical pathosis and were endodontically treated but despite all effort were non-restorable and had poor long-term prognosis. This case illustrates that extraction of all 4 PFM and a careful planed orthodontic treatment can be beneficial to the oral health of young patients.
Case History
An 11–year–old girl was referenced to the Department of Orthodontics from the residents of the Department of Pediatric Dentistry. All of her first permanent teeth were estimated as not restorable- although, root canal treatment was performed and some healing process was observed, the destruction of the crown was so advanced that the pediatric dentist could not provide durable restoration. All the roots were supererupted and there was no place for restoration.
Diagnosis
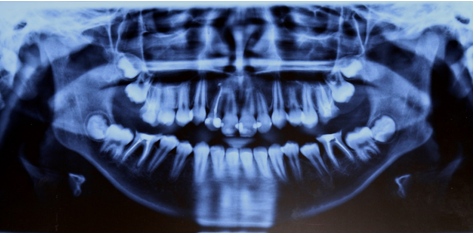
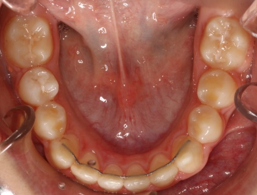
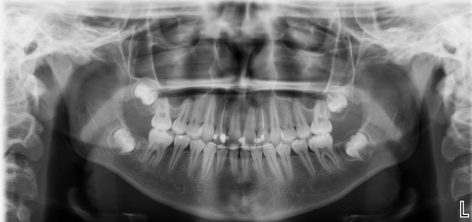
Initial record set was taken at 24.10.17. (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13) After full orthodontic examination it was found that the patient had severe skeletal Class II with ANB angle of 6,75 o, SNA = 86,42o,, SNB=79,66o; normodivergent (mesocephalic) facial pattern FMA= 29.58o; severe dental Class II molar relationship; large overjet =5.39mm; normal overbite; normal upper incisor inclination: U1/ FH= 111.49o, U1/SN=105,16o; proclined lower incisors IMPA=95,30o; normal interincisal angle 123,64o; normal upper incisal display; normal soft-tissue profile; all wisdom teeth were in place and in a reasonably good position; all second permanent molars had formed bifurcaions and trifurcations, and their roots were formed to ½ of their length. Teeth 26,36,46 still had signs of apical pathosis 6 months after the completion of the treatment. All first permanent molars had temporary fillings because the occlusion did not provide enough space for post and composite restoration or any other permanent restoration. The interdisciplinary team decided it was in the best interest of the patient to extract all first permanent molars because of their poor long-term prognosis. Because of the advanced stage of root length formation of the second permanent molars it was not to be expected that the extraction spaces would close on their own, and the accompanying orthodontic deformation made it necessary to start an orthodontic treatment one month after the extraction of the last first permanent molar. Treatment alternatives were explained to the patient and her parents, and they signed an informed consent.
Treatment objectives
Specific objectives of treatment: close extraction spaces with the patient‘s own teeth, achieve normal occlusion, normal overjet and resolve dental class II.
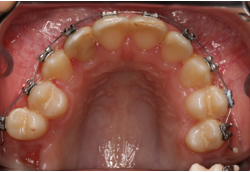
Treatment Plan and treatment progress : 022 MBT multibracket appliance was placed on 12.12.17. (Figure 14, Figure 15, Figure 16) In the first stage of the treatment all teeth were aligned, the scissors bite in the area of teeth 15 and 24 was resolved and normal occlusion was achieved. Intermaxilary crossbite elastics were used in the scissors bite correction. They were worn 24 hours per day for 4 months on both sides. Modified class II elastics were used for dental class II correction from lower second premolars to upper lateral incisors. They were worn 24 hours per day for 6 months on both sides. In this way, the anchorage for the second stage of treatment was prepared. The second stage started after the eruption of second permanent molars. The prepared dental arches were the anchorage needed for the second molar mesialization.
The molar mesialization was achieved with elastic chains while the rest of the teeth of the dental arch were held with 019x025 SS archwire so there was less torque loss. After molars were mesialized they were included in a 014 NiTi overlay arch that was engaged in all brackets. After molars were uprighted a rectangular 016x022 NiTi wire was put in place in both arches, and after that a 017x025 SS arch was placed. Vertical elastics were used for occlusion detailing.
On the 16.1.20 the treatment was completed and brackets were removed. The final set of records was taken and examined (Figure 17, Figure 18, Figure 19, Figure 20, Figure 21, Figure 22, Figure 23, Figure 24, Figure 25, Figure 26, Figure 27, Figure 28, Figure 29). In the lower jaw fixed retainer was placed on teeth 33,32,31,41,42,43, and in addition an Essix retainer was fabricated. In the upper jaw Essix retainer was placed. The patient was instructed to wear the retainers all day except when eating and brushing for the first 3 months, and after that, only through the night. Given the final positions of the second permanent molars, and the position of the third molars on the X-Ray the prognosis is good. During the treatment the patient went on regular dental check –ups with the pediatric dentist, who provided professional cleaning and motivation, and also protected the second permanent molars with fissure sealant in the time of their eruption.
Results
The treatment lasted 25 months. In the end of the treatment the panoramic X-ray showed that all teeth had parallel roots. Dental class I was achieved. The overjet and overbite were normal. The cephalometric analysis showed: ANB angle of 5.17 o, SNA = 85,48o, SNB=80.31; normodivergent (mesocephalic) facial pattern FMA= 29.28o; dental Class I molar and canine relationship; normal overjet =2.06 mm; normal overbite; upper incisor were retroclined U1/ FH= 103.72o, U1/SN=97,82o; lower incisors inclination was normal IMPA=91,03o; slightly upright interincisal angle 135,98o; normal upper incisal display; normal soft-tissue profile. Dental correction of the skeletal class II was achieved. One year after debonding, no clinically significant changes were noted in tooth positioning and the occlusion was stable, third molars were still not erupting. The compromised teeth were extracted and new stable positions of the second permanent molars were achieved. The future eruption of the third molars will allow this patient to have fully functional dentition with 28 teeth.
Discussion
The timing of first molar eruption makes these teeth susceptible to dental caries especially if the patient has a high caries risk. Both the general or pediatric dentist and the orthodontist should plan the treatment together. Besides the presenting clinical features, a number of additional factors may influence decision-making: social background, the need for general anesthetic for tooth extraction, the child‘s cooperation with restorative or orthodontic treatment, prevention and oral hygiene, difficulties in accessing restorative or orthodontic treatment.7 In the presented case the need for prolonged orthodontic treatment was not a favorable factor due to the high caries risk and the previous dental history of the patient. The patient compliance with the pediatric dentist was what granted the successful outcome of the treatment and no new carious lesions were found after the removal of braces.
The other important aspect of this kind of treatment is to consider the proper timing of FPM extraction. It depends on the following factors: upper or lower compromised FPM; type of malocclusion; extent of intra-arch crowding.3 Space gained from the bilateral extraction of the upper FPMs can be utilized for overjet reduction, correction of the Class II malocclusion and dental alignment.3 In the presented case dental correction of skeletal Class II deformation was achieved using some of the space provided from upper FPM extraction. The ideal time for lower FPM extraction has been estimated to be 8–9 years of age. 8 At this time, the crown of the lower second permanent molar is complete and the bifurcation of its roots is visible, and a maximum amount of spontaneous mesial movement can be expected. Even if a small space does remain between the second permanent molar and second premolar, this can be easily closed with fixed appliance therapy. In the presented case report the patient is 11- year old, and the second permanent molars, although, still not erupted in the mouth, were in more advanced stage of root formation. That is why maximum spontaneous space closure was not expected in this case and orthodontic treatment was necessary.
In cases when the optimal time has been missed or there are other orthodontic problems orthodontic treatment with fixed appliance can be beneficial. However, the treatment time may be significantly increased- FPM extraction usually increases the overall fixed appliance treatment time by 6–9 months. 9 The presented case confirmed this as the treatment lasted 25 months, but a significant part of this period second permanent molars were expected to erupt, and the total treatment time was determined by the time required to bring the lower second permanent molars into a satisfactory relationship with the lower second premolars.
The amount of intra-arch crowding can also affect the orthodontic space closure. Closing large residual spaces in the absence of significant crowding causes anterior segment retraction, and this negatively affects the soft tissue profile. This can complicate the treatment mechanics and temporary anchorage devices may be necessary to assist in the space closure and prevent unaesthetic consequences of anterior segment retraction. 3 In this case in the upper arch there was no significant crowding, and in the course of treatment the upper incisors were slightly over retracted. On one hand, this helped in achieving overjet reduction since in this patient the skeletal Class II relationship was due to the position of the maxilla. On the other hand, if mini implants were used in this case more effective torque control on the incisor teeth would have been possible. The profile of the patient was not affected, and an aesthetic final result was achieved.
Conclusion
Extraction of first permanent molars at a young age is a difficult decision, but it can be highly beneficial to the patient if it is done well. Therefore, it is recommended that a team of pediatric dentist and an orthodontist plan the treatment together as soon as possible after detection of a compromised FPM. Although, comprehensive orthodontic treatment may not be needed for a number of years in some cases, an orthodontic consultation can provide case-specific information with respect to the need and timing of FPM and other associated extractions.