- Visibility 4k Views
- Downloads 92 Downloads
- Permissions
- DOI 10.18231/j.ijodr.2020.044
-
CrossMark
- Citation
Temporary anchorage devices in orthodontics: A review
- Author Details:
-
Nausheer Ahmed
-
Rithika Joseph *
-
Abrar Younus A
-
K Ranjan R Bhat
Abstract
During orthodontic treatment it is crucial to prevent the unintentional movement of the anchorage unit whilst causing movement of other teeth. Conventional methods of anchorage control came along with many shortcomings. The introduction of skeletal anchorage in the form of temporary anchorage devices (TADs) or miniscrews has greatly benefited orthodontists in finding a way of anchorage control with minimum patient compliance and without a complicated clinical insertion and removal procedures. This review article outlines about the types of TADs, parts, techniques of insertion and removal and its clinical applications in orthodontics.
Introduction
“Secure Anchorage” is the primary requirement for successful treatment of various malocclusions.[1] conventionally, anchorage requirement for orthodontic tooth movement was provided by the teeth, extraoral and/or intermaxillary appliances.[2] These methods often have inadequate mechanical systems for anchorage control that leads to anchorage loss of reactive units and results in unfinished intra and interarch alignment. As an effort to eliminate this limitation, bulky acrylic appliances or extraoral appliances were intergrated by various clinicians but it resulted in poor patient compliance that contributed to loss of anchorage.[3] Any unwanted movement of the anchor teeth is called anchorage loss.[1] Absolute anchorage is defined as no movement of the anchorage units and can only be achieved by using ankylosed teeth or dental implants.[4] According to Cope, “A temporary anchorage device (TAD) is a device that is temporarily fixed to bone for the purpose of enhancing orthodontic anchorage either by supporting the teeth of the reactive unit or by obviating the need for the reactive unit altogether, and which is subsequently removed after use”.[3] Bone based anchorage units includes miniscrews and miniplates that are collectively called as temporary anchorage devices(TADs).[5]
Historical Outlook
Evolution of orthodontic implants was followed the development of dental implants and orthognathic fixation methods. These techniques were combined with basic biological and biomechanical principles of osseointegration. Earliest record of idea for skeletal anchorage was by Gainsforth and Higley (1945) who proposed possibilities of orthodontic anchorage in the basal bone by inserting Vitallium screws into a dog’s ramus for the purpose of distalising a maxillary canine. [6] The concept of osseointegration and use of titanium implants for replacement of teeth was introduced by Per Ingvar Branemark. [7], [8] Creekmore and Eklund (1983) gave the first clinical report of TAD usage in the anterior nasal spine for intrusion of upper incisors in a patient with severe deep bite. [9] Kanomi (1997) was the first to describe that mini implant of 1.2 mm diameter and 6 mm length can be explicitly used for orthodontic purpose. [10] Abso-Anchor Screw was developed in 1999 by a group of Korean clinicians, Aarhus Mini-Implant was created by a Scandinavian group and an Italian group developed The Spider Screw in 2003. Lately, palatal onplants, mid palatal screws and miniplate implants are being researched and reported. [11]
Classification
Labanauskaite et al [12] classified implants as following:
According to shape and size
a. Conical (cylindrical)
- Miniscrew implants
- Palatal implants
- Prosthodontic implants
b. Miniplate implants
c. Disk implants (onplants)
According to implant bone contact
a. Osseointegrated
b. Non-osseointegrated
According to the application
a. Orthodontic implants
b. Prosthodontic implants
The implantable anchorage devices can also be classified based on types of anchorage device used on the following bases
Endosseous implants [13]
These are osseointegrated implants that can withstand more mechanical force compared to the mechanically retaining implants. The drawbacks of this type is that there is a waiting period before loading, extensive surgical procedure is required for placement and the removal is problematic. These were used earlier in the palate for molar distalization.
Surgical miniplates- [3], [13]
The modified or conventional surgical titanium miniplates with intraoral extension can be used for orthodontic anchorage. Regions with thick cortical bone such as the zygomatic region and the buccal shelf area of the mandible are suitable for such implants. Applications of these implants include en masse molar distalization and intrusion of buccal segment in open bite cases. The downside of these implants was the need for extensive surgical procedure and post-operative discomfort for the patient.
Miniscrew implants (MSIs)
These implants have mechanical retention and provide short duration anchorage in orthodontics. The small diameter of these screws provides high versatility for placement site. Inter-radicular bone is the most common site for placement. These implants are absolute anchorage units.
Design and parts
Conventional MSI has the following parts
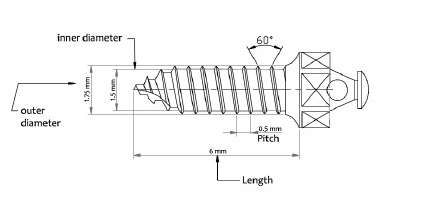
Head
It is the orally exposed portion of the screw which provides attachment for the springs and elastics. It has a screw driver slot or a particular design to engage the miniscrew driver for implant placement. Numerous kinds of head design are available for different types of anchorage and for prevention of soft tissue irritation. Most common type is the button like design with a sphere or double sphere-like shape or a hexagonal shape. A 0.8mm diameter hole in the head or neck of the screw is mostly used for direct anchorage. Furthermore, bracket-like designs are also available that can be used for both types of anchorage. [14] The driving head can only be used on the miniscrew given by that specific manufacturer. The head of the screw encompasses a hole and a collar for various attachments.[6] [Figure 1] shows the parts of a miniscrew.[15]
Neck
Screw neck or the trans-mucosal part passes through the mucosa and connects the screw with head. Variable lengths of neck are available for different mucosal thickness. The surface of the neck should be smooth and well-polished to diminish plaque accumulation around the neck. The junction of TAD with the mucosa is crucial as most of the implant failure due to peri-implantitis usually begins from this site.
Screw
This part gets embedded in the cortical or medullary bone to provide retention. The thread of the screw around shank or main body of the TAD has the cutting edge that facilitates insertion. The depth of the cutting edge and its angle determines the stresses generated during insertion and the amount of insertion torque required for insertion.
Thread design can be conical as in miniscrews or parallel tapering only at the end as in Orthodontic Mini Implant. [4] [Figure 2] shows different types of miniscrews. The length of TAD is defined as the length of the threaded body. It can range from 5-12mm for various clinical procedure according to anatomical considerations. [16] Costa et al evaluated the intraoral hard and soft tissue depths and established that miniscrew implants of 4-6mm length are safe in most regions, but subject to variations according to the bone depth of individual patients. [17] Total screw length id determined by the screw, neck and head length. The major diameter of TAD is the maximum diameter determined by the outer diameter of the threads and can range from 1.2 -2 mm. Diameters greater than 2mm should not be used in the inter-radicular region and those less than 1.2mm are weak and prone to breakage. [18] The minor diameter refers to the inner core diameter, which usually ranges from 0.2 to 1.6mm. The pitch of the screw is the distance between the two threads. High pitch denotes threads placed far apart and vice versa. A screw with a larger pitch gets inserted at a faster rate. [Figure 3] shows the design features of a miniscrew. [Table 1] shows the currently available orthodontic miniscrew systems.
|
Product |
Company |
Address |
|
Aarhus Anchorage System |
MEDICON eG ScanOrto A/S |
Tuttlingen, Germany. Charlottenlund, Denmark. |
|
AbsoAnchor System |
Dentos |
Taegu, Korea. |
|
C-Implant |
Dentium Inc. |
Seoul, Korea. |
|
Cizeta Titanium Miniscrew |
Cizeta Surgical |
Bologna, Italy. |
|
Dual-Top Anchor System |
Jeil Medical Corporation Distributed by RMO Inc. |
Seoul, Korea. Denver, Colorado. |
|
IMTEC Mini Ortho Implant |
IMTEC Corporation |
Ardmore, Oklahoma. |
|
Lin/Liou Orthodontic Mini Anchorage Screw (LOMAS) |
Mondeal Medical Systems GmbH Distributed by Mondeal North America, Inc. |
Tuttlingen, Germany. Comstock Park, Michigan. |
|
Miniscrew Anchorage System (MAS) |
Miscerium S.p.a. |
Avegno, Italy. |
|
Orthoanchor K1 System |
Dentsply Sankin Corporation |
Tokyo, Japan. |
|
Orthodontic Mini Implant (OMI) |
Leone S.p.A. Distributed by Leone America |
Firenze, Italy. |
|
Spider Screw Anchorage System |
HDC |
Sarcedo, Italy. |
|
Temporary Mini Orthodontic Anchorage System (TOMAS) |
Dentaurum |
Ispringen, Germany. |
|
Universal Skeletal Anchorage System |
Stryker Corporation |
Portage, Michigan. |
Properties [14]
Biocompatibility
Medical type IV or type V titanium alloy (Ti6Al4V) which is an alloy of titanium, aluminium and vanadium is the material of choice for the production of majority of the implants except for Orthodontic Mini Implants, which is made from stainless steel. The medical grade titanium offers biocompatibility and strength which is higher as compared with commercially pure (CP) titanium.
Osseointegration
TADs are designed to be mechanically retained in the bone. For easier removal of TADs, extensive osseointegration is detrimental. For this reason, these devices are made with smooth surfaces in order to reduce the bone ingrowth and to promote soft tissue attachment and without any special surface treatment regimen.
Types of anchorage
Two discrete types of anchorage can be provided by TADs. Direct anchorage implies that the implant receives the reactive forces directly by acting as an anchor unit. In indirect anchorage, bars or wires are used to attach the implant to the reactive unit. Although orthodontic mechanism requires not more than 300g force, TADs are designed to withstand up to 500g force. FEM studies indicate that direct loading may overload the TADs and the peri-implant bone leading to failure of TAD. [19], [20] Hence, indirectly loaded TADs is a healthy option in clinical situations where direct loading is not preferable. [21] [Figure 4], [Figure 5] shows direct anchorage and indirect anchorage respectively.





Indications for use of TADs
Absolute anchorage in maximum retraction requirements.
For patients not compliant with the use of headgear, TADs are viable option for anchorage.
In case of missing first molars, TADs can provide anchorage as well as help manage the space judiciously.
For difficult tooth movements such as anterior /posterior intrusion, en masse distalization of upper/lower arches, molar up righting and molar distalization.
In adult orthodontics for complex tooth movements.
TADs can also be used for the attachment of orthopaedic forces to jaws when there is a lack of anchorage units.
Correction of midline asymmetry and cant of occlusion.
Clinical Procedure
Case selection, informed consent and records
Patient’s medical history and assessment of oral cavity for absence of gingival inflammation and periodontal disease are to be done initially. Informed consent should always be obtained from the patient or the parent. Apart from the usual orthodontic records, intraoral radiographs of the proposed miniscrew site have to be taken to assess the bone morphology and roots of adjacent teeth. [22] In case further assessment of bone quality is required; cone beam computed tomography (CBCT) may be taken for bone density values. It has been suggested that D4 and D5 bones types are not suitable for implants. [23]
Sites of Insertion
In the maxilla, TADs can be placed in the incisive fossa, canine fossa, infra-zygomatic ridge, pre-maxillary region or mid-palatal region. While in the mandible, TADs can be placed in symphysis, canine fossa, anterior external oblique ridge, retro-molar area or sub-maxillary fossa. [17]
Studies have shown that the safest site for placement of TADs in the maxilla was in the anterior and apical portion and the tuberosity region was most unsuited for implant placement due to reduced bone thickness in this region. In the mandible, safest insertion site was between the first and second molars and between first and second premolars. [24] In the palate, the strongest bone support for implant insertion was found 6 to 9mm posterior to the incisive foramen and 3 to 6 mm paramedian. [25]
Placement of TADs in the extra-alveolar bone will diminish tooth root contact and allows the force vector closer to the centre of resistance of the tooth. But such implants will lay in mobile alveolar mucosa which can be overcome by using trans-mucosal attachments. [17]
Direction of Insertion
The miniscrew implants are inserted obliquely in an apical direction in the maxilla and parallel to the roots in the mandible. [26] In the maxilla, insertion angulation is 30° to 40° to the long axes of the teeth while it is 10° to 20° in the mandible. [27] In the region of maxillary sinus, a more perpendicular direction of insertion of mini implant is suggested to minimize the chances of perforation of maxillary sinus. [28]
Technique for Placement
The miniscrew implants can be self-drilling or self-tapping. An adjustable acrylic template or surgical guide can be used before implant placement. Recently, clinicians have used 3D CBCT, and customized surgical guide fabricated using stereolithographic techniques. This method helps for placement of self-drilling miniscrews with precision adjacent to dental roots and maxillary sinuses. [29], [30]
In self-tapping screws, predrilling is done under a small amount of local anaesthesia, preferably by an oral surgeon. At the site of placement, soft tissue is removed using a soft tissue punch and the pilot hole is drilled using a drill bit and a drill rotating at a speed not exceeding 1000rpm. The pilot hole should be maximum 2 to 3mm deep and should be 0.3mm smaller than the screw diameter. The implant is then inserted using an appropriate screw driver.
The self-drilling screws have specially formed tips and cutting flutes that can be inserted into the bone without predrilling, thereby decreasing the likelihood of damage to the tooth root, tooth germ or nerves, thermal necrosis of the bones and the fracture of the drill bit. [4] However, self-drilling screw requires pilot hole drilling if the thickness of bone cortex is more than 2mm which may cause the bending of the fine tip of the screw. [14] Figure 6 shows self-drilling and self-tapping screws.
Loading and anchorage consideration
Unlike dental implants immediate loading of orthodontic miniscrews can be done using light forces. [28] It is advisable to provide at least 2 mm clearance between the implant and the adjacent tooth root as the implant might move during orthodontic loading in some patients. [31]
Implant removal
The miniscrew can be removed using the same screw driver with or without local anaesthesia. Normally, the wound after implant removal does not require any special treatment and heals uneventfully. In case the screw cannot be retrieved during the removal appointment, it is advisable to wait for 3 to 4 days. The micro fractures or bone remodelling caused due to the initial attempt will loosen the screw. In case of implant fracture during removal, a small surgical procedure may be required for removal. [14]
Orthodontic Indications of TADs[4]
The absolute indication for TADs is high anchorage cases. It can also be used in cases where the dental units are quantitatively or qualitatively compromised, for asymmetric tooth movement along any plane and as a substitute for orthognathic surgeries to certain extent. In orthodontics, TADs have been used for various cases like:
Correction of deep bite
Extraction space closure
Canted occlusal planes and dental midline correction
Impacted canines alignment
Up-righting and extrusion of impacted molars
Intrusion of molars
Maxillary molar distalization and distalization of mandibular teeth
Molar mesialization
En masse retraction of anterior teeth
Correction of vertical skeletal discrepancies.
Risk Factors [1]
It can be classified as:
1. General risk factors – good general health is essential for uneventful healing and prevention of inflammation around the implant. General risk factors include tobacco smoking, age, [32], [33] risk of infective endocarditis, diabetes and medications like bisphosphonates, immune-modulators, anti-epileptics and anticoagulants.
2. Local risk factors – it includes gingivitis and periodontitis, reduced mouth opening, bone quality and radiotherapy.
Complications [34]
Complications during insertion – Inter-radicular miniscrew placement can cause trauma to root of the tooth and periodontal ligament. Slippage of the miniscrew under the mucosal tissue along the periosteum may occur due to failure to completely engage the cortical bone. Nerve injury during miniscrew insertion is higher in the maxillary palatal slope, the mandibular buccal dentoalveolus and the retromolar area. Air subcutaneous emphysema may result during miniscrew placement through the loose alveolar tissue in the retromolar, mandibular posterior buccal and zygomatic region. Perforation of the nasal sinus and maxillary sinuses may occur during insertion in the maxillary incisal, maxillary posterior dentoalveolar and zygomatic region. Miniscrew stability may be disturbed due to increased torsional stresses during placement causing implant bending or fracture or micro fractures in the peri-implant bone.
Complications under orthodontic loading – Stationary anchorage failure may occur due to low bone density and inadequate cortical bone thickness. Miniscrew migration within the bone is potential as absolute anchorage under orthodontic loading is not always achievable.
Soft tissue complications include aphthous ulceration, soft tissue overgrowth on miniscrew head and auxiliary, soft tissue inflammation, infection and peri-implantitis.
Complications during removal comprise miniscrew fracture and partial osseointegration.
Limitations of TADs
Orthodontic implants are contraindicated in case of systemic bone diseases and in medically compromising conditions. Patients younger than 12 years of age who have not yet completed the skeletal growth are inappropriate for TAD placement. Miniscrews should not be placed adjacent to bone remodelling areas such as healing socket or near a deciduous tooth. Thin cortical bone less than 0.5mm is a limitation for miniscrew placement. Clinician’s skill is a key factor for implant usage. Ethical issues due to the invasive nature of the procedure are a restraint.
Conclusion
Temporary Anchorage Device is a strong aid for the orthodontist in resolving many challenges faced during tooth movement. Despite the limitations like root injuries, peri-implantitis and implant failure, the advantages of easier insertion and removal technique, immediate loading and absolute anchorage gives TADs a very important place in orthodontics. A thorough knowledge about the factors affecting the success of mini implants will benefit in achieving desired treatment results with minimal patient chair-side time.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Hoste S, Vercruyssen M, Quirynen M, Willems G. Risk factors and indications of orthodontic temporary anchorage devices: a literature review. Aust Orthod J. 2008;24(2):140-8. [Google Scholar]
- Schätzle M, Männchen R, Zwahlen M, Lang NP. Survival and failure rates of orthodontic temporary anchorage devices: a systematic review. Clini Oral Implants Res. 2009;20(12):1351-9. [Google Scholar] [Crossref]
- Cope J. Temporary Anchorage Devices in Orthodontics: A Paradigm Shift. Semin Orthod. 2005;11:3-9. [Google Scholar]
- Kalra A, Jaggi N, Jasoria G, Shamim W, Rathore S, Manchanda M. Miniscrew Implants as Temporary Anchorage Devices in Orthodontics: A Comprehensive Review. J Contemp Dent Pract. 2013;14(5):993-9. [Google Scholar] [Crossref]
- Mizrahi E. The use of miniscrews in orthodontics: A review of selected clinical applications. Prim Dent J. 2016;5(4):20-7. [Google Scholar]
- Gainsforth B, Higley L. A study of orthodontic anchorage possibilities in basal bone. Am J Orthod Oral Surg. 1945;31(8):406-17. [Google Scholar] [Crossref]
- Brånemark P, Aspegren K, Breine U. Microcirculatory Studies in Man By High Resolution Vital Microscopy. Angiol. 1964;15(8):329-32. [Google Scholar] [Crossref]
- Brånemark P, Breine U, Adell R, Hansson BO, Lindström J, Ohlsson �. Intra-Osseous Anchorage of Dental Prostheses:I. Experimental Studies. Scand J Plast Reconstr Surg. 1969;3(2):81-100. [Google Scholar] [Crossref]
- Creekmore TD, Eklund MK. The Possibility of Skeletal Anchorage. J Clin Orthod. 1983;17:266-9. [Google Scholar]
- Kanomi R. Mini implant for orthodontic anchorage. J Clin Orthod. 1997;31:763-70. [Google Scholar]
- Mizrahi E, Mizrahi B. Mini-screw implants (temporary anchorage devices): orthodontic and pre-prosthetic applications. J Orthod. 2007;34(2):80-94. [Google Scholar] [Crossref]
- Labanaaskaite B, Jankauskas G, Vasiliauskas A, Haffar N. Implants for orthodontic anchorage. Meta-analysis. Stomatol. 2005;7:128-32. [Google Scholar]
- Roberts WE, Helm FR, Marshall KJ, Gongloff RK. Rigid endosseous implants for orthodontic and orthopedic anchorage. Angle Orthod. 1989;59(4):247-56. [Google Scholar]
- Papadopoulos MA, Tarawneh F. The use of miniscrew implants for temporary skeletal anchorage in orthodontics: A comprehensive review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod . 2007;103:e6-e15. [Google Scholar] [Crossref]
- AM, WN. Miniscrews: Clinical Application of Orthodontic. RRJDS. 2014;2(3):32-43. [Google Scholar] [Crossref]
- Suzuki M, Deguchi T, Watanabe H, Seiryu M, Iikubo M, Sasano T. Evaluation of optimal length and insertion torque for miniscrews. Am J Orthod Dentofacial Orthop . 2013;144(2):251-9. [Google Scholar] [Crossref]
- Costa A, Pasta G, Bergamaschi G. Intraoral hard and soft tissue depths for temporary anchorage devices. Semin Orthod. 2005;11(1):10-5. [Google Scholar] [Crossref]
- SSL, Cruz-Marroquin E, Sun J, Stewart KT, Allen MR. Orthodontic mini-implant diameter does not affect in-situ linear microcrack generation in the mandible or the maxilla. Am J Orthod Dentofacial Orthop . 2012;142(6):768-73. [Google Scholar] [Crossref]
- Holberg C, Winterhalder P, Holberg N, Rudzki-Janson I, Wichelhaus A. Direct versus indirect loading of orthodontic miniscrew implants—an FEM analysis. Clin Oral Investig. 2013;17(8):1821-7. [Google Scholar] [Crossref]
- Holberg C, Winterhalder P, Holberg N, Wichelhaus A, Rudzki-Janson I. Indirect miniscrew anchorage: biomechanical loading of the dental anchorage during mandibular molar protraction—an FEM analysis. J Orofac Orthop. 2014;75(1):16-24. [Google Scholar] [Crossref]
- Purmal K, Alam MK, Pohchi A, Razak NHA. 3D Mapping of Safe and Danger Zones in the Maxilla and Mandible for the Placement of Intermaxillary Fixation Screws. PLoS ONE. 2013;8(12). [Google Scholar] [Crossref]
- Fayed MMS, Pazera P, Katsaros C. Optimal sites for orthodontic mini-implant placement assessed by cone beam computed tomography. Angle Orthod. 2010;80(5):939-51. [Google Scholar] [Crossref]
- Chen Y, Chang H, Lin H, Lai EH, Hung ., Yao H. Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Implants Res. 2008;19(11):1188-96. [Google Scholar]
- Poggioa PM, Incorvati C, Velo S, Carano A. Safe Zones’’: A Guide for Miniscrew Positioning in the Maxillary and Mandibular Arch. Angle Orthod. 2006;76:191-7. [Google Scholar]
- Bernhart T, Vollgruber A, Gahleitner A, Dörtbudak O, Haas R. Alternative to the median region of the palate for placement of an orthodontic implant. Clin Oral Implants Res. 2000;11(6):595-601. [Google Scholar] [Crossref]
- Melsen B. Mini-implants. Where are we?. J Clin Orthod. 2005;39:539-47. [Google Scholar]
- Kyung HM, Park HS, Bae SM, Sung JH, Kim IB. Development of orthodontic micro-implants for intraoral anchorage. J Clin Orthod. 2003;37:321-8. [Google Scholar]
- Carano A, Velo S, Leone P, Siciliani G. Clinical applications of the miniscrew anchorage system. J Clin Orthod. 2005;39:9-24. [Google Scholar]
- Miyazawa K, Kawaguchi M, Tabuchi M, Goto S. Accurate pre-surgical determination for self-drilling miniscrew implant placement using surgical guides and cone-beam computed tomography. Eur J Orthod. 2010;32(6):735-40. [Google Scholar] [Crossref]
- Kim SH, Kang JM, Choi B, Nelson G. Clinical application of a stereolithographic surgical guide for simple positioning of orthodontic mini-implants. World J Orthod. 2008;9(4):371-82. [Google Scholar]
- Liou EJ, Pai BC, Lin JC. Do miniscrews remain stationary under orthodontic forces?. Am J Orthod Dentofac Orthop. 2004;126(1):42-7. [Google Scholar] [Crossref]
- Moon C, Lee D, Lee H, Im J, Baek S. Factors Associated with the Success Rate of Orthodontic Miniscrews Placed in the Upper and Lower Posterior Buccal Region. Angle Orthod. 2008;78(1):101-6. [Google Scholar]
- Viwattanatipa N, Thanakitcharu S, Uttraravichien A, Pitiphat W. Survival analyses of surgical miniscrews as orthodontic anchorage. Am J Orthod Dentofac Orthop. 2009;136(1):29-36. [Google Scholar] [Crossref]
- Kravitz ND, Kusnoto B. Risks and complications of orthodontic miniscrews. Am J Orthod Dentofac Orthop. 2007;131(4):S43-S51. [Google Scholar] [Crossref]
- Abstract
- Introduction
- Historical Outlook
- Classification
- The implantable anchorage devices can also be classified based on types of anchorage device used on the following bases
- Design and parts
- Properties [14]
- Clinical Procedure
- Case selection, informed consent and records
- Sites of Insertion
- Direction of Insertion
- Technique for Placement
- Loading and anchorage consideration
- Implant removal
- Orthodontic Indications of TADs[4]
- Risk Factors [1]
- Complications [34]
- Limitations of TADs
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Ahmed N, Joseph R, A AY, Bhat KRR. Temporary anchorage devices in orthodontics: A review [Internet]. IP Indian J Orthod Dentofacial Res. 2020 [cited 2025 Oct 01];6(4):222-228. Available from: https://doi.org/10.18231/j.ijodr.2020.044
APA
Ahmed, N., Joseph, R., A, A. Y., Bhat, K. R. R. (2020). Temporary anchorage devices in orthodontics: A review. IP Indian J Orthod Dentofacial Res, 6(4), 222-228. https://doi.org/10.18231/j.ijodr.2020.044
MLA
Ahmed, Nausheer, Joseph, Rithika, A, Abrar Younus, Bhat, K Ranjan R. "Temporary anchorage devices in orthodontics: A review." IP Indian J Orthod Dentofacial Res, vol. 6, no. 4, 2020, pp. 222-228. https://doi.org/10.18231/j.ijodr.2020.044
Chicago
Ahmed, N., Joseph, R., A, A. Y., Bhat, K. R. R.. "Temporary anchorage devices in orthodontics: A review." IP Indian J Orthod Dentofacial Res 6, no. 4 (2020): 222-228. https://doi.org/10.18231/j.ijodr.2020.044
