- Visibility 149 Views
- Downloads 18 Downloads
- DOI 10.18231/j.ijodr.2020.033
-
CrossMark
- Citation
Rhinoplasty, septoplasty and genioplasty with fixed orthodontic mechanotherapy for non-surgical correction of a patient with “Long face syndrome” Having a class III malocclusion on a class II skeletal jaw base - A case report
- Author Details:
-
Bhushan Jawale
-
Lishoy Rodrigues *
-
Kiran Shinde
-
Suresh Kangane
-
Rohan Hattarki
Introduction
Long face syndrome is a relatively common feature among many orthodontic patients. Classical features include an increased lower facial height, anterior open-bite and a narrow palate. While excessive vertical facial growth can often be recognized clinically, several cephalometric traits are commonly used to classify the underlying vertical skeletal pattern as normodivergent, hypodivergent or hyperdivergent.[1] The term “long face syndrome” depicts only the vertical component of the three dimensional problem which exists in these patients. [2] Etiological factors such as enlarged adenoids, nasal allergies, weak masticatory muscles, oral habits, and genetic factors have all been implicated in the development of the long face morphology.[3] Orthognathic surgery is the treatment indicated in most cases to correct this malformation. The intervention may include the following isolated or combined strategies: maxillary impaction, chin reduction, or anti-clockwise rotation of the occlusal plane. The treatment for young patients troubled by long face syndrome is to halt and control descent of the lower jaw and to prevent the eruption of posterior teeth. In severe cases of deformity, a mixture of orthodontics and orthognathic surgery may be the only effective solution. [4] When you breathe through the mouth, the muscles in the cheeks have to work harder and become taut. [5] The more frequently you breathe through the mouth, the greater the influence of these forces, which eventually can narrow the shape of the face as well as the dental arches
Case Report
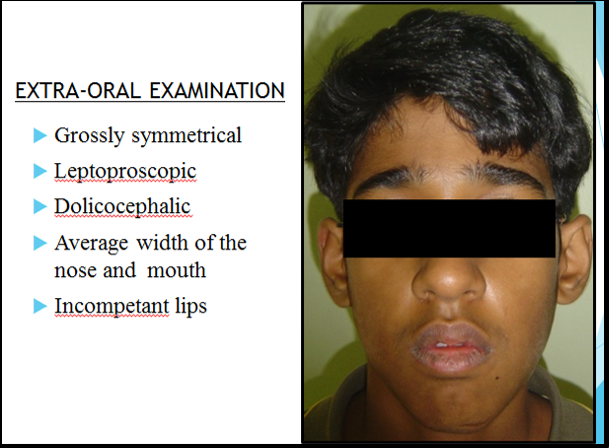
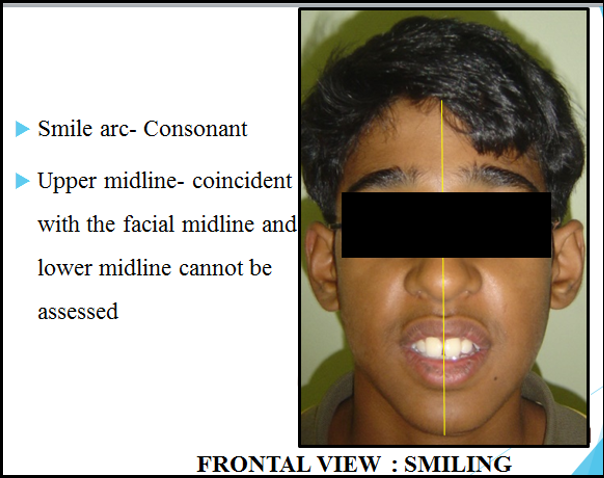
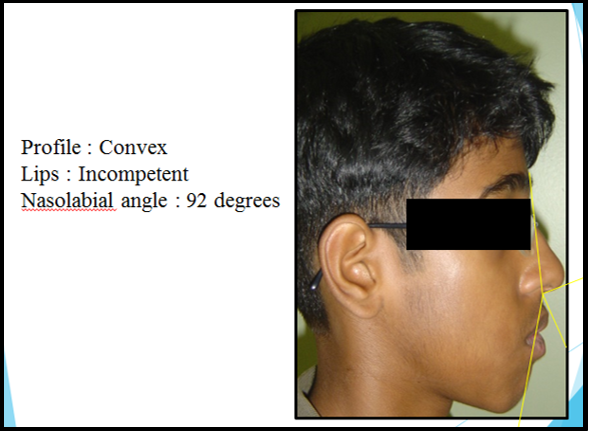
Extra-oral examination
A 16 year old male patient presented with the chief complain of excessive show of upper front teeth and also increased lower anterior facial height. On Extra-oral examination, the patient had a convex facial profile, slightly asymmetrical face with the chin deviated towards the left of the patients face, incompetent lips, shallow mento-labial sulcus and a reduced Nasolabial Angle, a Leptoprosopic facial form, Dolicocephalic head form, average width of nose and mouth, minimal buccal corridor space, a consonant smile arc and slightly posterior divergence of face . The patient had no relevant prenatal, natal, postnatal history or a family history. However the patient presented with a history of difficulty while breathing due to a deviated nasal septum and presence of nasal polyps. Also, on frontal view, the patient showed the presence of increased lower anterior facial height with a “Long Face Syndrome”. On Smiling, there was complete show of maxillary anterior teeth with show of upper gums. However, mandibular teeth were not visible on smile. The patient had a gummy smile, an unaesthetic smile arc and was very dissatisfied with his smile.

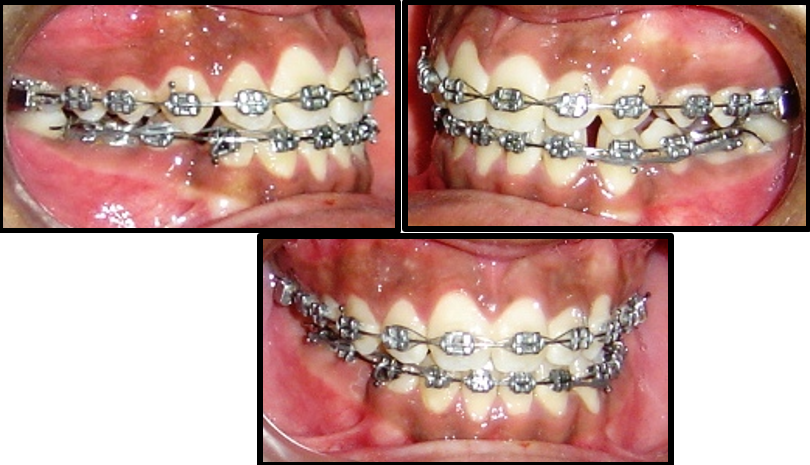
Intra-oral examination
Intraoral examination on frontal view showed presence of an edge to edge bite with spaced upper anterior region and mildly crowded lower anterior region. On lateral view the patient showed the presence of Class III incisor relationship, a Class III Canine relationship on both sides and a Class III molar relationship bilaterally. Patient had an overjet of 0 mm and an overbite of 0mm.The upper and lower arch shows the presence of a V shaped arch form and there was a cross-bite present between 24 and 35. The patient also showed presence of a lateral open bite bilaterally.

Photographic analysis
| Parameters | Pre- treatment |
| SNA | 83° |
| SNB | 80° |
| ANB | 3° |
| WITS | 3mm(AO ahead of BO) |
| MAX. LENGTH | 76mm |
| MAN. LENGTH | 109mm |
| IMPA | 99° |
| NASOLABIAL ANGLE | 92° |
| U1 TO NA DEGREES | 35° |
| U1 TO NA mm | 6mm |
| L1 TO NB DEGREES | 29° |
| L1 TO NB mm | 5mm |
| U1/L1 ANGLE | 119° |
| SADDLE ANGLE | 132° |
| ARTICULAR ANGLE | 144° |
| GONIAL ANGLE | 142° |
| FMA | 38° |
| Y AXIS | 70° |
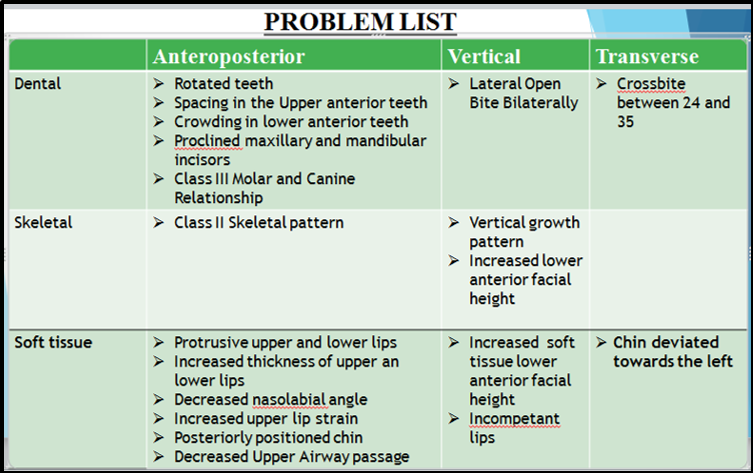
Diagnosis
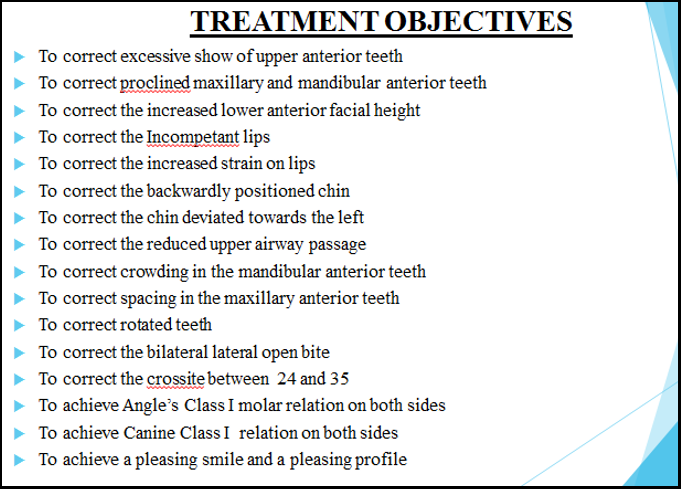
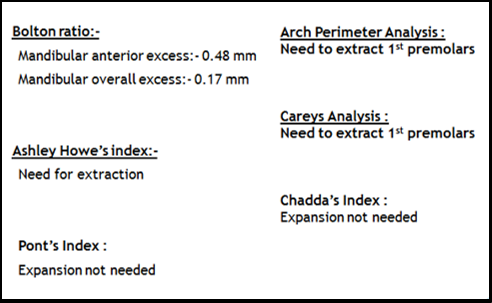
This 16 years old Male patient was diagnosed with Long Face Syndrome, a Class II skeletal pattern, Angle’s Class III malocclusion with a vertical growth pattern, an increased lower anterior facial height of both hard and soft tissue, a backwardly positioned chin and a deviated chin position towards the left of patients face, a bilateral lateral open bite and a cross-bite between 24 and 35, with a skeletally increased upper and lower, both anterior and posterior dental height with proclined upper and lower incisors, crowding in lower anterior region, spacing in the upper anterior region, rotated teeth, increased lip strain, protrusive upper and lower lips , increased thickness of upper and lower lips, incompetent upper and lower lips, with a reduced Nasolabial angle with a reduced upper pharyngeal airway space.
Treatment progress
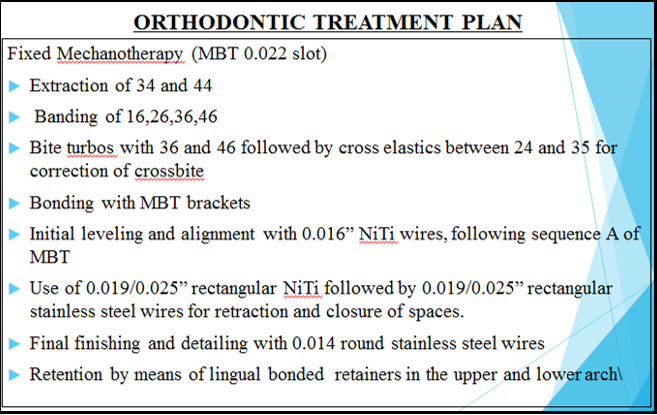
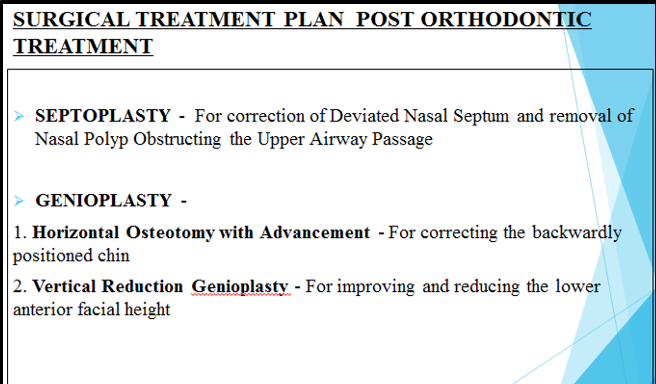
The mandibular 1st premolars were extracted. Complete banding was done with all molars followed by placement of bite turbos on the mandibular 1st molars bilaterally for bite opening and provided clearance for correction of cross-bite. Cross elastics were then given between 24 and 35 until the cross-bite was corrected. Thereafter bonding in both maxillary and mandibular arch was done using MBT 0.022X0.028”slot. Initially a 0.012” NiTi wire was used which was followed by 0.014”, 0.016”, 0.018”, 0.020” NiTi archwires following sequence ‘A’ of MBT. After 6 months of alignment and leveling, NiTi round wires were discontinued. The existing lateral open bite was consequently corrected. Use of 0.019” x 0.025” rectangular NiTi with accentuated Anchor sweeps in the upper and lower stiff arch wires were given to prevent the bite deepening during retraction in the lower arch followed by 0.019” x 0.025” rectangular stainless steel wires for retraction of closure of spaces. Finally light settling elastics were given with rectangular steel wires in lower arch and 0.012” light NiTi wire in upper arch for settling , finishing, detailing and proper intercuspation. The crowded dentition in lower anterior region was unraveled, spacing and irregularity of upper anterior region was closed and aligned respectively and the incisor relationship changed from Class III to Class I .Canine relationship also changed from Class III to Class I, however, Molar relation was ended in Class III. Hawley’s removable retainers were given to the patient followed by fixed lingual bonded retainers in the upper and lower arch. After completion of orthodontic treatment, elective minor surgical procedures like Rhinoplasty, Septoplasty and Genioplasty were carried out to improve the breathing pattern of the patient, correct the nasal contour, correct the backwardly positioned chin and also to reduce the increased chin height of the patient respectively. Both Septoplasty and Polyp removal were performed using Non Invasive FESS (Functional Endoscopic Sinus Surgery). After these elective minor surgical procedures, the smile of the patient changed from being unaesthetic to a more pleasing one. The treatment changed the patients overall profile and helped him feel more confident. He was very happy and satisfied with the treatment. The entire treatment lasted for 18 months.



| Parameters | Post-treatment |
| SNA | 82° |
| SNB | 80° |
| ANB | 2° |
| WITS | 1mm |
| Max. Length | 78mm |
| Man. Length | 108mm |
| IMPA | 92° |
| Nasolabial Angle | 99° |
| U1 TO NA DEGREES | 28° |
| U1 TO NA mm | 3mm |
| L1 TO NB DEGREES | 24° |
| L1 TO NB mm | 2mm |
| U1/L1 ANGLE | 132° |
| Saddle angle | 128° |
| Articular angle | 142° |
| Gonial angle | 135° |
| FMA | 32° |
| Y AXIS | 67° |

Discussion
While excessive vertical facial growth can often be recognized clinically, several cephalometric traits are commonly used to classify the underlying vertical skeletal pattern as normodivergent, hypodivergent or hyperdivergent. [1] The term “long face syndrome” depicts only the vertical component of the three dimensional problem which exists in these patients.[2] Etiological factors such as enlarged adenoids, nasal allergies, weak masticatory muscles, oral habits, and genetic factors have all been implicated in the development of the long face morphology. [6], [7] Orthognathic surgery is the treatment indicated in most cases to correct this malformation. [8] Before the Orthodontist can determine the optimal treatment, he or she must consider the contributing factors. These include normal growth and development, tooth size discrepancies, excessive incisor vertical overlap of different causes, mesiodistal and labiolingual incisor angulation, generalized spacing and pathological conditions.[9] A carefully developed differential diagnosis allows the practitioner to choose the most effective orthodontic and/or restorative treatment. [10], [11] Treatment of a patient with long face syndrome with increased lower anterior facial height is challenging. A well-chosen individualized treatment plan, undertaken with sound biomechanical principles and appropriate control of orthodontic mechanics to execute the plan is the surest way to achieve predictable results with minimal side effects.[3] A patient with Long Face Syndrome might have any number of a combination of the skeletal and dental components. Hence, identifying and understanding the etiology and expression of Vertical Growth with a long face and increased lower anterior facial height and identifying differential diagnosis is helpful for its correction.[12], [4] The patient's chief complaint was excessive show of upper front teeth and also increased length of the lower face. The selection of orthodontic fixed appliances is dependent upon several factors which can be categorized into patient factors, such as age and compliance, and clinical factors, such as preference/familiarity and laboratory facilities. The execution of only Fixed appliance therapy and extraction of lower 1st premolars appropriately resulted in an improvement in the patient's profile in this case. Alongside fixed orthodontic treatment, the mandibular 1st premolars were removed and retraction was done to correct the already existing malocclusion of an edge to edge bite to a proper molar intercuspation along with ideal incisor and canine relationship. This patient had a very unique malocclusion. He had a Class III Dental relationship on a Class II Skeletal Base. The patient presented with spacing in the upper anterior region and crowding in the lower anterior region with an edge to edge incisor relationship due to which it was decided to extract the lower 1st premolars and rectify the malocclusion. A lateral open bite was present initially which got corrected consequently during fixed appliance therapy. The U1 to NA values both in degrees and in mm decreased. Successful results were obtained after the fixed MBT appliance therapy within a stipulated period of time. The overall treatment time was 16 months. After this active treatment phase, the profile of this 16 year old male patient improved significantly as seen in the post treatment Extra-oral photographs. Removable Hawley’s retainers followed by fixed lingual bonded retainers were then delivered to the patient. The crowding in the lower arch and spacing in the upper arch was corrected and the smile arc of the patient improved drastically to being more consonant and pleasant. After the orthodontic fixed appliance therapy, 2 minor surgeries were carried out. Firstly the patient had difficulty in breathing due to obstructed upper airway passage. He showed presence of a deviated nasal septum and Nasal polyps which hindered his breathing pattern drastically. Mc Namara analysis clearly was indicative of a compromised upper pharyngeal airway space on analysis of the Lateral Cephalogram. Hence, Septoplasty was carried out for correction of the Deviated Nasal Septum and the nasal polyp was excised. Thereafter Rhinoplasty was carried out for changing and reshaping the contour of the nose. Both Septoplasty and Polyp removal were performed using Non Invasive FESS (Functional Endoscopic Sinus Surgery). The 2nd chief complain of the patient was an increased lower anterior facial height. Now this could be possibly be corrected only by means of surgery, however, we decided to proceed ahead without execution of any major surgeries for the correction of the same as it was against the will of the patient. Therefore a minor surgical procedure of Genioplasty was carried out for recontouring of the chin, firstly to advance it forward and also at the same time to reduce its height, thus addressing the chief complaint of the patient of having an increased lower facial height. The Genioplasty was carried out in 2 steps. First, a horizontal Osteotomy with Advancement, for correcting the backwardly positioned chin. Second, a Vertical Reduction Genioplasty for reducing and correcting the lower anterior facial height of the patient. Alongside this procedure the chin was placed slightly towards the right coincident with the facial midline as the patient had a deviated chin towards the left before treatment. The Profile of the patient drastically changed at the end of the treatment within 18 months and the patient was very happy and satisfied with the results.
| Parameters | Pre- treatment | Post-treatment |
| SNA | 83° | 82° |
| SNB | 80° | 80° |
| ANB | 3° | 2° |
| WITS | 3mm(AO ahead of BO) | 1mm |
| Max. Length | 76mm | 78mm |
| Man. Length | 109mm | 108mm |
| IMPA | 99° | 92° |
| Nasolabial angle | 92° | 99° |
| U1 TO NA DEGREES | 35° | 28° |
| U1 TO NA mm | 6mm | 3mm |
| L1 TO NB DEGREES | 29° | 24° |
| L1 TO NB mm | 5mm | 2mm |
| U1/L1 ANGLE | 119° | 132° |
| Saddle angle | 132° | 128° |
| Articular angle | 144° | 142° |
| Gonial angle | 142° | 135° |
| FMA | 38° | 32° |
| Y AXIS | 70° | 67° |
Conclusion
This case report shows how the correction of a long face syndrome patient can be achieved alongside fixed orthodontic treatment without the need for major surgical procedure and merely by executing simplified elective surgical procedures, thus bringing about and enabling drastic changes in the patients overall profile and appearance. The planned goals set in the pretreatment plan were successfully attained. Treatment of this case included the extraction of mandibular 1st premolars followed by retraction with a resultant profile improvement. Furthermore the profile and appearance of the patient improved more after performing minor elective surgical procedures like Septoplasty, Genioplasty and Rhinoplasty. The maxillary and mandibular teeth were found to be esthetically satisfactory in the line of occlusion with a pleasing consonant smile arc. The overjet was near ideal and normal overbite was achieved. The correction of the malocclusion was achieved, with a significant improvement in the patient aesthetics and self-esteem. Duration of treatment was 18 months. The patient was very satisfied with the results of this comparatively lesser invasive surgical treatment.
Source of Funding
None.
Conflict of Interest
None.
References
- Viken Sassouni. A classification of skeletal facial types. Am J Orthod 1969. [Google Scholar]
- Stephen A. Schendel, Jerome Eisenfeld, William H. Bell, Bruce N. Epker, David J. Mishelevich. The long face syndrome: Vertical maxillary excess. Am J Orthod 1976. [Google Scholar]
- J R Isaacson, R J Isaacson, T M Speidel, F W Worms. Extreme variation in vertical facial growth and associated variation in skeletal and dental relations. Angle Orthod 1971. [Google Scholar]
- A. R. Collett, V. C. West. Terminology of facial morphology in the vertical dimension. Aust Dent J 1993. [Google Scholar]
- Cedric A. Quick, Karsten K. H. Gundlach. Adenoid facies. Laryngoscope 1978. [Google Scholar]
- W R Proffit, C Phillips, C T Dann. Who seeks surgical-orthodontic treatment?. Int J Adult Orthodon Orthognath Surg 1990. [Google Scholar]
- L J Bailey, L H Haltiwanger, G H Blakey, W R Proffit. Who seeks surgical-orthodontic treatment: a current review. Int J Adult Orthodon Orthognath Surg 2001. [Google Scholar]
- K. Willmar. On Le Fort I Osteotomy. A Follow-up Study of 106 Operated Patients with Maxillo-Facial Deformity. Dentomaxillofac Radiol 1975. [Google Scholar]
- P P Siriwat, J R Jarabak. Malocclusion and facial morphology is there a relationship? An epidemiologic study. Angle Orthod 1985. [Google Scholar]
- G. Willems, I. De Bruyne, A. Verdonck, S. Fieuws, C. Carels. Prevalence of dentofacial characteristics in a Belgian orthodontic population. Clin Oral Investig 2001. [Google Scholar]
- Eloísa Marcantonio Boeck, Nádia Lunardi, Ary dos Santos Pinto, Karina Eiras Dela Coletta Pizzol, Rodolfo Jorge Boeck Neto. Occurrence of skeletal malocclusions in Brazilian patients with dentofacial deformities. Braz Dent J 2011. [Google Scholar]
- F F Schudy. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod 1964. [Google Scholar]
How to Cite This Article
Vancouver
Jawale B, Rodrigues L, Shinde K, Kangane S, Hattarki R. Rhinoplasty, septoplasty and genioplasty with fixed orthodontic mechanotherapy for non-surgical correction of a patient with “Long face syndrome” Having a class III malocclusion on a class II skeletal jaw base - A case report [Internet]. IP Indian J Orthod Dentofacial Res. 2020 [cited 2025 Sep 12];6(3):170-176. Available from: https://doi.org/10.18231/j.ijodr.2020.033
APA
Jawale, B., Rodrigues, L., Shinde, K., Kangane, S., Hattarki, R. (2020). Rhinoplasty, septoplasty and genioplasty with fixed orthodontic mechanotherapy for non-surgical correction of a patient with “Long face syndrome” Having a class III malocclusion on a class II skeletal jaw base - A case report. IP Indian J Orthod Dentofacial Res, 6(3), 170-176. https://doi.org/10.18231/j.ijodr.2020.033
MLA
Jawale, Bhushan, Rodrigues, Lishoy, Shinde, Kiran, Kangane, Suresh, Hattarki, Rohan. "Rhinoplasty, septoplasty and genioplasty with fixed orthodontic mechanotherapy for non-surgical correction of a patient with “Long face syndrome” Having a class III malocclusion on a class II skeletal jaw base - A case report." IP Indian J Orthod Dentofacial Res, vol. 6, no. 3, 2020, pp. 170-176. https://doi.org/10.18231/j.ijodr.2020.033
Chicago
Jawale, B., Rodrigues, L., Shinde, K., Kangane, S., Hattarki, R.. "Rhinoplasty, septoplasty and genioplasty with fixed orthodontic mechanotherapy for non-surgical correction of a patient with “Long face syndrome” Having a class III malocclusion on a class II skeletal jaw base - A case report." IP Indian J Orthod Dentofacial Res 6, no. 3 (2020): 170-176. https://doi.org/10.18231/j.ijodr.2020.033
