Introduction
The mental foramen (MF) is found on the lateral aspect of the body of mandible. It marks the termination of mandibular canal in the mandible through which the inferior alveolar nerve and vessels pass, and transmits mental nerves and vessels. The mental bundle passes through the MF and supplies blood supply and sensory innervations to the soft tissues of the lower lip, chin, and gingival tissue on the ipsilateral side of the mandible.1 Any foramen additionally to mental foramen within the body of mandible is known as accessory mental foramen (AMF).2
The vertical location of the MF varies according to age. It is located closer to the alveolar crest before tooth eruption in children, and located precisely at 13 to 15mm superior to inferior border of mandible in adult. 3 Some authors studied the horizontal position of MF and found that 65% of MFs were present between the second premolar and first molar. 4 but others reported that it is present in the line with long axis of second premolar 5 or between the first and second premolar. 3 All standard radiological and anatomical text books contain conflicting statements regarding the location and shape of MF.6 The variations are largely influenced by gender, age, individual, race, degree of alveolar bone resorption and type of technique used.7
Studying location, size and shape of MF is important to localize the important maxillofacial neurovascular bundle. They act as the important anatomical landmark for the local anesthetic, surgical, or other invasive procedures for dental surgeons performing any surgical procedure in the mental region of the mandible. 8 Cone beam computed tomography (CBCT) enables us to accurately determine the location, shape, and size of the MF as well as the presence of AMF, and allows for an accurate morphometric analysis, and also provides life-size images where precise lines and measurements can be made easily. 9 The aim of the present research was to study the anatomical characteristic of the MF using CBCT in selected dentate adult patients of Kashmir region, to determine the shape, position with respect to adjacent teeth, distances to the apex of mandibular premolars and lower border of the mandible, in relation to the gender and age of the patient. The CBCT images were analysed for the presence of any accessory mental foramen.
Materials and Methods
The CBCTs of dentate adult patients of both sexes, above or equal to 16 years of age, and fulfill the inclusion criteria were gathered from the Orthodontic Department of the Government Dental College Srinagar, taken as part of diagnosis and treatment planning. All the CBCT scans were taken by Newtom Giano CBCT 3D imaging (QRsr 1 Verona, Italy). The following settings were used:
Ray source: HF, Constant potential (DC, 90 kV; 2 mA (pulsed
Imaging mode: CBCT
Focal spot: 0.5 mm
Dose: 80-100 µSv
Scan : 11 cm × 8 cm and 8 cm × 8 cm
Scan time: 18 seconds
Software: NNT™ with free viewer and sharing application.
All CBCT images were of dentate patients and had the following inclusion criteria:
All mandibular teeth from the right first molar to the left first molar were present, with no orthodontic appliance, supernumerary teeth, periodontal diseases, mandibular dental irregularity, or spaces between teeth.
The images were free from any radiolucent or radiopaque lesion in the lower arch.
CBCT images of patients with the following criteria were excluded:
Pathology that affected the position of MF and other adjacent landmarks, patients had undergone a previous mandibular surgical procedure or with a history of mandibular fracture.
Any missing mandibular teeth from the right first molar to the left first molar to avoid the possibility of teeth drifting towards the missing tooth space.
Patients in which the upper premolars were missing because of the possibility of over eruption of the lower premolars.
All measurements were made by a single observer in oblique sagittal plane. For assessment of intra-observer reliability and reproducibility, CBCT measurements of 21 patients were repeated twice. No statistically significant difference was detected. All analyses were studied and all the data were compared between the gender and age for each measurement and information. The parameters measured and studied were as follows:
Shape of MF: The shape of mental foramen was determined as oval, round or irregular (Figure 1).
Accessory mental foramina: The three dimensional images were looked for the presence of any accessory mental foramina (Figure 1).
Figure 1
3D CBCT image for determining the shape of MF and looking for the presence of any accessory mental foramina.

Position of MF: Horizontal position of the MF on the radiograph was recorded, and for more precise location of MF, the vertical midline of the foramen was considered as a standard point to locate the foramen horizontally as follows.10:
P1: The foramen situated anterior to the first premolar.
P2: The foramen situated in line with the first premolar.
P3: The foramen situated between the first and second premolar.
P4: The foramen situated in line with second premolar.
P5: The foramen situated between the second premolar and first molar (Figure 2).
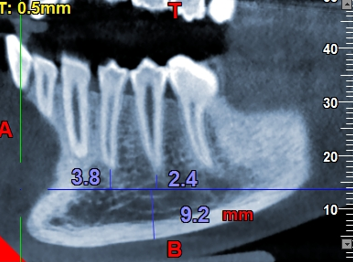
Distance of MF: The horizontal midline passing through the middle of MF was used as a reference line of measurement; to measure the vertical distance of the MF from the inferior border of mandible, and from the apices of mandibular first and second premolars (Figure 2).
Statistical analysis
The statistical analysis of data was carried with the help of means, ranges and standard deviations.
Student’s t-test and ANOVA test was used to test the difference between means of various variables. A P-value of less than 0.05 was considered statistically significant. Statistical package SPSS (Version 20.0) was used to carry out the statistical analysis of data.
Based on the normalcy of the distribution of the data, results obtained were statistically analyzed and compared using SPSS software. The statistical analysis included:
Results
The MFs were studied on the CBCT images of 31 patients. There were 13 males (mean age 37.15 years) and 18 females (mean age 34.11 years). The age ranged from 16 to 60 years with a total mean of 35.4 years. Only one case (3.2%) was seen associated with AMF (Figure 3).
Shape of MF: The round shape was most frequent (67.7%), followed by oval shape (19.3%) and the least was irregular (12.9%).
Position of MF:
A. Horizontal: In males and females and in every age group studied, the most frequent horizontal position was (P3) in which the foramen situated between the first and second premolar (35.5%), followed by (P4) in which the foramen situated in line with second premolar (32.3%). P5 position in which the foramen situated distal to second premolar was found in 16.1% of the studied group and P1 position in which the foramen situated mesial to the first premolar in 9.7%. P2 position in which the foramen situated in line with the first premolar was found in only 6.5% of the studied group (Table 1).
Table 1
Horizontal position of mental foramen
B. Vertical: The mean vertical distance from the apex of 1st premolar to the MF was 5.61±2.09mm, from the apex of 2nd premolar to the MF was 5.97±2.33mm, and from the MF to the inferior border of the mandible was 10.11±2.33mm (Table 2). Table 3 and 4 shows the gender and age comparision for the vertical measurements of the mental foramen.
Table 2
Showing Vertical measurements of mental foramen
Table 3
Showing gender comparision for vertical measurements of mental foramen
| Male N = 13 | Female N = 18 | P-value | |
| Distance from 4 | 5.15 ±2.407 | 5.93 ±1.835 | 0.311 |
| Distance from 5 | 5.66 ±2.842 | 6.18 ±1.947 | 0.544 |
| Distance from inferior border | 10.94 ±2.293 | 9.50 ±2.219 | 0.088 |
Table 4
Showing age comparision for vertical measurements of mental foramen (ANOVA test)
Discussion
After reviewing the literature regarding anatomical, morphometric analysis and the relations of MF to important landmark in the mandible based on CBCT, no any research present regarding all these detailed data about MF in a Kashmiri population. So the MFs in the present study were determined on the CBCT images of 31 patients with a mean age of 35.4±4.32 years.
Accessory mental foramen (AMF)
Only one (3.2%) was seen associated with AMF. Sekerci et al. found that AMFs were seen in 2% of the cases.9 Ilayperuma et al. and Kalender et al. found it was present in 3.92% and 6.5% of the cases studied respectively. 11, 12 Khojastepour et al. found that AMF present in 5.1% of the cases studied. 13 These results disagree with that of Juan and Eduardo, they found that AMFs were found in 55.5% of the cases studied.14 Sawyer et al. 15 reported Ethnic variation in relation to AMF.
Shape of MF
The round shape represents the highest percentage in the present study (67.7%). Sekerci et al. and Al-Khateeb et al. have also found the predominance of round shape in their study. 9, 16 Sheikhi et al. 1 Juan and Eduardo, 14 Chu et al 17 and Muinelo-Lorenzo et al. 18 have reported the oval shape to be the most commonly found. Fabian found that the round and oval shapes were reported to gain nearly equal percentages in Tanzanian populations. 19
Horizontal position
The most frequent horizontal position was P3 followed by P4. Statistically a nonsignificant difference between MF horizontal position and gender was seen. Sheikhi et al. and Al-Juboori et al. found that the most common horizontal locations of MFs were positions P3 followed by P4, and no significant difference between the horizontal locations of MF and gender, mean age and side were seen. 1, 20 Haghanifar et al. study in Iranian population, and Rupesh et al. study in Indian population also showed that the most frequent location of the mental foramen was position P3, but followed by positions P4. 3, 21
Al Jasser and Nwoku did a study on Saudi population using panoramic radiographs and found that MF is most commonly positioned at P4 and the location of mental foramen was not gender dependent.10 Sekerci et al. found that in males the most frequent horizontal position of the MF was P4, and in females was P3, and found that with advancing age there was a decrease in the frequency of more posterior locations of the MF.9 Juan and Eduardo found that the most frequent location of the MF in Perú population was P4, followed by positions P5, P3, and P2, and no mental foramen was found in position P1, and a nonsignificant difference present between both sides. 14 Khojastepour et al. found that most MFs studied are present in line with second premolar in selected Iranian population, and in none of the cases the MF was located at P1 or P6 (MF situated in line with first molar). 13 Muinelo-Lorenzo et al. found that 57.9 % of MFs studied in Spain population was situated in P4 position, and 25.3% of MF was situated in P3 position, and P6 showed the lowest percentage. 18 The variations in the results could be attributed to ethnic or race differences.22 Some authors found that MF is positioned more posteriorly to the second premolar in blacks than in whites. 23
Distance (Vertical position)
In the present study, the distances from the apex of 1st and 2nd mandibular premolar to the centre of mental foramen (V1 & V2), and from the centre of mental foramen to the inferior border of mandible (V3) was measured for each patient; and mean values were calculated. The mean values for V1, V2 and V3 were 5.61±2.09mm, 5.97±2.33mm and 10.11±2.33mm, respectively (Table 2). V3 distance was less in females than males and the difference was statistically non-significant (Table 3).
This may be due to gender differences in mandible size. V3 distance was more in older age group, perhaps due to bone resorption. Other authors found no influence of age on this distance. 24 The differences between studies may be due to the differences in the method used, they study the MFs in dentate, partially dentate and edentulous patients.
The ideal image for the mental foramen would be a three dimensional image having very high spatial resolution at low exposures. This can be achieved with Cone Beam Computed Tomography (CBCT), which makes it an ideal form of imaging and allows for precise understanding of the relationship between structures in an anatomically complex area.25
The use of periapical or panoramic radiographs can be limited due to focal plane shape, projection geometry, vertical over or under angulation, horizontal angulation, and faulty patient position.26, 27 Due to these limitations and advances in technology, CBCT has gained popularity and acceptance in all fields of dentistry.28 CBCT when used for measuring mandibular anatomy has shown to have an error of less than 0.6%.29
Due to the importance of the location of the mental foramen when planning for dental surgical procedures, the lack of agreement on the location, size and orientation, and the advances in CBCT, a more updated study of the foramen was initiated. The purpose of this study was to use existing CBCT images to determine the vertical and horizontal location of the mental foramen in relation to the mandibular first and second premolars, as well as the distance in millimeters from the apex of each. The distance from the foramen to the inferior border of the mandible was also recorded.
The study also illustrates that sex and age can have some significance on the position of the foramen. These trends are particularly clear for the location of the foramen in relation to the inferior border of the mandible and in its horizontal position. The foramen is distinctly farther away from the inferior border of the mandible in male and older patients. An average increase of 0.0885mm per year of patients’ age is seen. Based on the significant differences between sexes regarding the distance of mental foramen to the inferior border of the mandible, the measurement may be useful in identifying the sex of human mandibles in the field of forensics.
There is a tendency for greater distal positioning of the foramen in female patients and in older patients. And, the foramen of older patients have a trend toward greater apical positioning in relation to the mandibular first premolar.
Considering the increased distal and apical positioning of the mental foramen seen to occur as age increases one would hypothesize that the foramen must move as people age. The prevailing thought from numerous growth studies over the last century was that facial skeletal growth stopped soon after puberty.30 However, recent studies have shown continued facial skeletal growth through adulthood.30, 31, 32, 33 As we age, the overall length of the mandible, as well as the body and ramus, increases. Males have more of a downward and forward movement, while females move straight down.31 The height of the mandible increases 2.5 ± 2.0mm through adulthood, with new bone deposited at the inferior border.33 Addition of this bone throughout adulthood explains the greater distance between the mental foramen and the inferior border of the mandible as patients age. The increase in the height of the mandible may also explain the greater apical position of the foramen as the foramen moves with the bone while the teeth stay relatively constant with the unchanged mandibular plane.33 Longitudinal studies would need to be undertaken to determine if the foramen moves with age in any one person.
The distalization of the foramen relative to the apices of the first premolar may be a consequence of the constant mesial migration of teeth. Cephalometric tracings from early adulthood throughout life show a distinct mesial migration of teeth.30, 33 Another study showed even patients with congenitally missing third molars exhibit distinct mesial crowding over time due to mesial migration.32
Conclusion
Statistical analysis showed no significant relation present with the gender and age group. Knowing the exact location of the mental foramens and its variations is very important and can help to plan surgical procedures properly. It can help in safe placement of mini-implants and temporary anchorage devices (TADS) for orthodontic skeletal anchorage in the lower jaw. The detailed information about the shape, position, distance and diameter of MF, and the relationship between MF and peripheral structures can help surgeons to localize the MF, avoid injury to neurovascular bundles, and to facilitate surgical, local anesthetic, and other invasive surgical procedures.
These results and their comparisons to the existing research show that the position of the mental foramen is not a fixed and predictable location. It also indicates that age and gender can have an effect on the location of the foramen. Since the foramen does not have any static and dependable landmarks, it is the responsibility of every practitioner to gain an understanding of the mental foramen’s location with adequate imaging prior to initiating surgical intervention, and thus reducing the risk of surgical sequelae.
CBCT technology offers valuable information regarding the mental foramen. Clinicians should carefully investigate the anatomy of the mental foramen, as well as the presence of accessory mental foramina before any mini-implant or temporary anchorage device (TAD) is placed in the mandibular premolar and molar area.