- Visibility 140 Views
- Downloads 16 Downloads
- Permissions
- DOI 10.18231/j.ijodr.2021.011
-
CrossMark
- Citation
Ortho-surgical management of class iii malocclusion: A case report
- Author Details:
-
Shilpa Kalra *
-
Ashish Kalra
-
Tripti Tikku
-
Kamna Srivastava
-
Rohit Khanna
Abstract
Class III malocclusion is considered to be one of the most difficult and complex orthodontic problems to treat. Prevalence of class III malocclusion in Caucasians ranges from 0.8 to 4.0% and rises up to 1213% in Chinese and Japanese populations, while in North Indian population, class III malocclusion is found in up to 3.4% of the population. A 19 years old boy who reported with chief complaint of poor smile because of forwardly placed lower jaw from 2 years. Treatment plan of orthodontic treatment first and surgery later was planned. The upper and lower arches were aligned until a 0.019” x 0.025” stainless steel archwire could be placed. . Bilateral sagittal split osteotomy with short lingual split was carried out using surgical saws. 05 mm set back of mandible was performed. After 06 weeks class III elastics and settling elastics were given.
Introduction
Class III malocclusion is considered to be one of the most difficult and complex orthodontic problems to treat. Prevalence of class III malocclusion in Caucasians ranges from 0.8 to 4.0% and rises up to 1213% in Chinese and Japanese populations, while in North Indian population, class III malocclusion is found in up to 3.4% of the population.[1] The features of Class III malocclusion patients may be short anterior cranial base, short and retrusive maxilla, proclined maxillary incisors, retroclined mandibular incisors.[1]
These complex cases require careful treatment planning, an integrated approach and patient cooperation.[2] A poor facial appearance is often the patient's chief complaint, but it may be accompanied by functional problems, temporomandibular disorders, or psychosocial handicaps.[3] Now a day’s shift is occurring towards viewing the patient as co decision maker. Ackerman says that we should “talk with” rather than “talk to” the patient. 2D imaging software and 2 D printing has made the process of diagnosis, treatment planning and patient involvement in their treatment much simpler, more accurate, acceptable and reliable for both Orthodontist and patient.[4]
Treatment modalities in Orthodontics include growth modification procedures in growing children, Orthodontic camouflage and Ortho surgical procedures in non-growing individuals. Combined treatment of Orthodontics with surgery had been the only answer to achieve the desired predictive results in adults with severe skeletal discrepancy.[5]
In this case report a 19 yrs old boy was treated with ortho-surgical method for management of class III malocclusion.
Case Report
A19 years old boy who reported with chief complaint of poor smile because of forwardly placed lower jaw from 2 years. Extra oral examination revealed, patient was well built, mesomorphic boy with symmetrical face, mesoprosopic facial form and incompetent lips with 1mm of mandibular incisors exposure at rest. On lateral examination, the mandibular prognathism with obtuse nasolabial angle were noted [Fig 1].
Intraorally patient was having posterior cross bite wrt upper posteriors on left side and premolars and 1st molar on right side. Both the arches were U shaped with rotated molars in upper arch and premolar rotation in lower arch with reverse overjet of 1 mm and 0.5 mm of overbite with bilateral class III molar and canine relation. The deviation of 1.5 mm midline to left side was also present [Fig 2].
To know about the quality and quantity of skeletal discrepancy, cephalogram tracing was done using manual method and Nemoceph software and values of Steiner’s, COGS and Arnett analysis were interpreted [[Table 1], [Table 2], [Table 3]]. Cephalometric findings revealed retrognathic maxilla sagittally and normal vertically and prognathic mandible with horizontal growth pattern. Maxillary central incisors were both protruded and proclined whereas mandibular central incisors were retroclined.
Treatment plan
Considering the extent of skeletal discrepancy, amount of reverse overjet and chief complaint, the treatment plan to correct the skeletal class III malocclusion by doing Orthodontic treatment initially followed by mandibular set back surgery later (FOSLA) was made. With the aim of achieving facial aesthetics and optimal functional occlusion, surgical treatment was planned. The objective was to achieve ideal occlusal relationships, in terms of canine class, molar relationship, overjet, overbite, and matching dental midlines.[4]
After performing a scaling, treatment was begun with 0.022” × 0.028” Roth system. The upper and lower arches were aligned using 0.016” followed by 0.020” Niti wire followed by rectangular Niti of 0.017” x 0.025” and 0.019”x 0.025” until a 0.019” x 0.025” stainless steel archwire could be placed [Fig 3]. The mandibular incisors were decompensated by proclining them in normal inclination and the arch forms were coordinated.
Prediction of the final outcome was done using predictive tracing by both manual and computerized methods.[5], [6] The value for mandibular set back as predicted using both the methods was 5 mm. Following this, a model mock surgery was done for visualizing 3-dimensional post-operative relationship of jaws with positive overjet and class I molar relation [][Figure 4] . The surgical stent was made at this position.
Surgical procedure
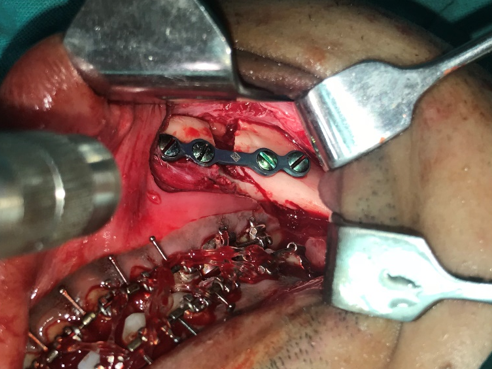
Surgery was performed with the support of oral & maxillofacial surgeons. Retromolar area was exposed, bilateral sagittal split osteotomy with short lingual split was done using surgical burs. Medial pterygoid muscle was detached after performing the split, 5 mm setback was achieved and rigid fixation was placed in the mandible through the use of four-hole miniplates on both sides [[Figure 5]]. To keep the mandible in the correct position, the use of intermaxillary elastics for 30 days were given to achieve maximum stability. The patient was under observation after the procedure and was guided subsequently to perform opening and lateral movements. Active orthodontic treatment was resumed four weeks after surgery. Class III and settling elastics were given. Six months later, fixed appliances were removed and a retention appliance was delivered [[Figure 6]].





|
Steiner’s |
Mean |
Indians |
Manual tracing Pre |
Nemoceph Tracing Pre |
Inference |
|
SNA |
82 |
82.28 |
80 |
81.6 |
|
|
SNB |
80 |
78.52 |
84 |
84.1 |
Prognathic mandible |
|
ANB |
2 |
3.52 |
- 4 |
-2.5 |
Class III skeletal Pattern |
|
SND |
76 |
|
77 |
84.3 |
|
|
Mx l to NA |
4mm/22 |
5.65/23.17 |
7mm/43 |
5.7/33.9 |
Proclined Maxillary Central incisors |
|
Md l to NB |
4mm/25 |
6.02/27.80 |
3.5mm/20 |
4.4/19.6 |
Retroclined mandibular incisors |
|
Pog to NB |
0mm |
|
3mm |
2.6 |
Prognathic mandible |
|
Pog-NB:Md l-NB |
1:1 |
|
3:3.5 |
2.6:4.4 |
|
|
OP to SN |
14.5 |
|
10 |
23.2 |
|
|
Go-GN to SN |
32 |
26.83 |
29 |
30.4 |
Horizontal Grower |
|
U1 to SN |
104+ 7 |
104.8 |
122 |
|
Proclined maxillary CI |
|
U1 to FH |
107 |
|
133 |
|
Proclined maxillary CI |
|
Measurements |
Mean + SD (Male) |
Mean + SD (Female) |
Manual Tracing Pre |
Nemoceph Tracing Pre |
Inference |
|
Cranial Base |
|
|
|
|
|
|
Ar-Ptm(II HP) |
37.1 +2.8 mm |
32.8 +1.9 mm |
30 mm |
28.6 |
|
|
PTM-N (II HP) |
52.8 +4.1 mm |
50.9 +3.0 mm |
55 mm |
51.6 |
Increased ant cranial base length |
|
Horizontal (Skeletal) |
|
|
|
|
|
|
N-A-Pg (Angle) |
3.9 + 6.40 |
2.6 + 5.10 |
-12 |
-7.6 |
Protruded mandible |
|
N-Pg (II HP) |
-4.3 + 8.5 mm |
-6.5 + 5.1 mm |
5.5 |
8.3 |
|
|
Vertical (Skeletal, Dental) |
|
|
|
|
|
|
N-ANS (I HP) |
54.7 + 3.2 mm |
50.0 + 2.4 mm |
51 |
49 |
|
|
ANS-Gn (I HP) |
68.6 + 3.8 mm |
61.3 + 3.3 mm |
66 |
64.3 |
|
|
PNS-N (I HP) |
53.9 + 1.7 mm |
50.6 + 2.2 mm |
52 |
50.5 |
|
|
U1-NF (I NF) |
23.0 + 5.9 mm |
27.5 + 1.7 mm |
25 |
23.6 |
|
|
L1-MP (I MP) |
30.5+ 2.1 mm |
40.8 + 1.8 mm |
37 |
37.4 |
|
|
U6-NF (I NF) |
45.0 + 2.1 mm |
23.0 + 1.3 mm |
21 |
23.6 |
Decreased Maxillary posterior vertical height |
|
L6-MP (I MP) |
26.2 + 2.0 mm |
32.1 + 1.9 mm |
32 |
30.4 |
Increased mandibular posterior vertical height |
|
Maxilla- Mandible |
|
|
|
|
|
|
PNS-ANS(II HP) |
57.7 + 2.5 mm |
52.6 + 3.5 mm |
54 |
|
|
|
Ar-Go (Linear) |
52.0 + 4.2 mm |
46.8 + 2.5 mm |
50 |
47.1 |
|
|
Go-pog (Linear) |
83.7 + 4.6 mm |
74.3 + 5.8 mm |
84 |
80.5 |
|
|
B-Pg (II MP) |
8.9 + 1.7 mm |
7.2 + 1.9 mm |
4 |
8.5 |
|
|
Ar-Go-Gn (Angle) |
119 + 6.50 |
122 + 6.90 |
1250 |
126.8 |
|
|
Dental |
|
|
|
|
|
|
OPUpper-HP (Angle) |
|
|
|
|
|
|
OP lower-HP (Angle) |
6.2 + 5.10 |
7.1 + 2.50 |
4 |
14.3 |
|
|
A-B (II OP) |
-1.1 + 2.00 |
-0.4 + 2.50 |
60 |
14.5 |
|
|
U1-NF (Angle) |
110.0 + 4.70 |
112.5 + 5.30 |
130 |
122.9 |
|
|
L1- MP (angle) |
95.9 + 5.20 |
95.9 + 5.70 |
92 |
83.7 |
|
|
Facial Form |
Mean |
Manual Tracing Pre |
Nemoceph Tracing Pre |
|
|
Facial convexity angle (G-Sn-Pg’) |
120 |
90 |
10.1 |
Concave Profile |
|
Maxillary Prognathism (G-Sn) (II HP) |
6 mm |
10 mm |
10 |
|
|
Mandibular Prognathism (G-Pg) (II HP) |
0 mm |
-7 mm |
-8.6 |
Mandibular prognathism |
|
Vertical height ratio (G-Sn/Sn-Me) (I HP) |
1 |
1.04 |
1 |
|
|
Lower face- throat angle (Sn-Gn’-C) |
1000 |
950 |
86.2 |
|
|
Lower vertical height- depth ratio (Sn-Gn’/C-Gn’) |
1.2 |
1.11 |
1.3 |
|
|
Lip position and facial form |
|
|
|
|
|
Nasolabial angle (Cm-Sn-Ls) |
1020 |
1150 |
114 |
|
|
Upper Lip Protrusion (Ls to Sn-Pg’) |
3 mm |
0.5 |
0.6 |
|
|
Lower Lip Protrusion (Li to Sn-Pg’) |
2 mm |
-2 |
-3.5 |
|
|
Mentolabial sulcus (Si to Li-Pg’) |
4 mm |
3.5 |
-4.2 |
|
|
Vertical Lip- Chin ratio (Sn-Stms/ Stmi-Me’) |
0.5 |
-0.4 |
-0.5 |
|
|
Maxillary Incisor exposure |
2 mm |
0 |
0.7 |
|
|
Interlabial Gap (Stms-Stmi) |
2 mm |
2 |
2.9 |
|
|
Measurement |
Mean |
Manual Tracing Pre |
Nemoceph Tracing Pre |
Inference |
|
Dentoskeletal Factors |
|
|
|
|
|
Mx1 projection to TVL |
-9.2mm |
-12 |
-13 |
|
|
Mx1 inclination (Mx1-Mx OP) |
56.80 |
47 |
53.6 |
Protruded maxillary incisor |
|
Overjet |
3.2 mm |
-2 |
-2.5 |
Prognathic mandible |
|
Md1 projection to TVL |
-12.4 mm |
-10 |
-11 |
Prognathic mandible |
|
Md1 inclination (Md1-Md OP) |
64.30 |
72 |
77 |
|
|
Overbite |
3.2 mm |
0.5 |
-1.7 |
|
|
Post height (Mx OP-TVL angle) |
95.6 mm |
91 |
92 |
|
|
Mx1 exposure relaxed lip |
4.7 mm |
2 |
0.7 |
|
|
Soft Tissue thickness |
|
|
|
|
|
Upper lip (UL inside –ULA) |
12.6 mm |
12 |
12.3 |
|
|
Lower lip (LL inside- LLA) |
13.6 mm |
12.5 |
14.7 |
|
|
Pogonion-chin (Pg-Pg’) |
11.8 |
9 |
9.7 |
Shows decreased soft tissue thickness over chin area |
|
Menton (Me-Me’) |
7.4 mm |
5.5 |
6.6 |
|
|
Facial height or length |
|
|
|
|
|
Upper lip length (Sn –ULI) |
21 mm |
17 |
21.6 |
|
|
Interlabial gap (ULI-ULS) |
0.0 mm |
2 |
1.3 |
|
|
Upper incisor exposure relaxed lip |
4.7 mm |
2 |
0.7 |
|
|
Lower lip length (LLS-Me’) |
46.9 mm |
48 |
46.2 |
|
|
Lower 1/3 height |
71.1 mm |
72 |
69.1 |
|
|
Total facial height (N’-Me’) |
124.6 mm |
122 |
118.8 |
|
|
Maxillary height (Sn-Mx1 tip) |
25.7 mm |
24 |
22.2 |
|
|
Mandibular Height(Md1 tip-Me’) |
48.6 mm |
46 |
38 |
|
|
Post height (Mx-OP-TVL angle) |
95.6 mm |
91 |
92 |
Decreased posterior maxillary height |
|
True vertical line projections |
|
|
|
|
|
Glabella (G’-TVL) |
--18.6 mm |
-10.5 |
-10 |
|
|
Soft Tissue A point (A’-TVL) |
-0.1 mm |
-3 |
-2.5 |
|
|
Upper incisor tip (Mx1-TVL) |
-9.2 |
-12 |
-13 |
|
|
Upper lip anterior (ULA-TVL) |
3.7 mm |
0 |
0.2 |
|
|
Upper lip angle (UL-TVL) |
12.10 |
-.9 |
0.8 |
|
|
Nasolabial angle (Cm-Sn-ULA) |
103.50 |
112 |
114.7 |
|
|
Lower incisor tip (Md1-TVL) |
-12.4 mm |
-10 |
-11 |
Shows uprighting of mandibular incisors |
|
Lower lip anterior (LLA-TVL) |
1.9 mm |
3.5 |
3.9 |
|
|
Soft tissue B point (B’-TVL) |
-5.3 mm |
-4 |
-3 |
|
|
Soft tissue pogonion (Pog’-TVL) |
-2.6 mm |
-0.5 |
-1.4 |
Mandibular prognathism |
|
Throat length (NTP-Pog’) |
58.2 mm |
58 |
56.9 |
|
|
Harmony values |
|
|
|
|
|
Facial Angle (G’-Sn-Pog’) |
169.30 |
172 |
169.9 |
|
|
Forehead to maxilla (G’-A’) |
8.4 mm |
16 |
7.5 |
|
|
Forehead to mandible (G’-Pog’) |
5.9 mm |
20 |
8.6 |
Prognathic mandible |
|
Nasal Base to chin (Sn-Pog’) |
3.2 mm |
7 |
1.4 |
|
|
Max base – Md base (A’-B’) |
5.2 mm |
5 |
0.6 |
|
|
Upper lip-lower lip (ULA-LLA) |
1.8 mm |
6 |
3.7 |
|
|
Incisor tip anterior to chin (Md1 tip-Pog’) |
9.8 mm |
-15 |
-11.6 |
|
|
Lower lip anterior –chin (LLA-Pog’) |
0.0 mm |
0 |
5.3 |
|
|
Chin Contour (B’-Pog) |
0.0 mm |
4 |
1.6 |
|
Discussion
When the skeletal or dentoalveolar deformity is so severe that the magnitude of the problem lies outside the envelop of possible correction by Orthodontics alone and even the camouflage is also not the option then Orthognathic surgery is the best plan. [4]
This case report describes the treatment of a boy with dental and skeletal class III relationships. In this case ortho- surgical treatment was the best option for achieving good esthetic result and an acceptable occlusion. Presurgical orthodontics involves removal of all the dental compensations and also suggests the extent of skeletal discrepancy. [1] With osteotomy and setback of the prognathic mandible, normal skeletal base relationship is achieved. Postsurgical orthodontics involves the normal occlusal rehabilitation.
Conclusion
A careful prediction and treatment planning are mandatory prior to planning for an Orthognathic case. A multidisciplinary team approach ensures a satisfactory and acceptable outcome.
Source of Funding
No financial support was received for the work within this manuscript.
Conflicts of interest
The author declares that they do not have any conflict of interests.
References
- Katiyar R, Singh GK, Mehrotra D, Singh A. Surgical orthodontic treatment of class III malocclusion. Natl J Maxillofac Surg. 2010;1(2):143-9. [Google Scholar]
- Phillips C, Proffit WR, WP, RJW, DS. Psychosocial aspects of dentofacial deformity and its treatment. Contemporary Treatment of Dentofacial Deformity. 2003. [Google Scholar]
- Bailey LJ, Sarver DM, Turvey TA, Proffit WR, Proffit WR, WP, et al. Contemporary Treatment of Dentofacial Deformity. . 2003. [Google Scholar]
- Kalra S, Tikku T, Khanna R, Maurya R, Verma S, Srivastava K. Prediction in an ortho surgical case: A report. Int J Orthod Rehab. 2019;10(1):42-8. [Google Scholar] [Crossref]
- Epker B, Fish L. Dentofacial deformities, Intergrated orthodontic and Surgical Correction. 2nd Edn.. 1980;II. [Google Scholar]
- Chen SK, Chen YJ, Yao CC, Chang HF. Enhanced speed and precision of measurement in a computer-assisted digital cephalometric analysis system. Angle Orthod. 2004;74:501-7. [Google Scholar]
How to Cite This Article
Vancouver
Kalra S, Kalra A, Tikku T, Srivastava K, Khanna R. Ortho-surgical management of class iii malocclusion: A case report [Internet]. IP Indian J Orthod Dentofacial Res. 2021 [cited 2025 Sep 22];7(1):62-67. Available from: https://doi.org/10.18231/j.ijodr.2021.011
APA
Kalra, S., Kalra, A., Tikku, T., Srivastava, K., Khanna, R. (2021). Ortho-surgical management of class iii malocclusion: A case report. IP Indian J Orthod Dentofacial Res, 7(1), 62-67. https://doi.org/10.18231/j.ijodr.2021.011
MLA
Kalra, Shilpa, Kalra, Ashish, Tikku, Tripti, Srivastava, Kamna, Khanna, Rohit. "Ortho-surgical management of class iii malocclusion: A case report." IP Indian J Orthod Dentofacial Res, vol. 7, no. 1, 2021, pp. 62-67. https://doi.org/10.18231/j.ijodr.2021.011
Chicago
Kalra, S., Kalra, A., Tikku, T., Srivastava, K., Khanna, R.. "Ortho-surgical management of class iii malocclusion: A case report." IP Indian J Orthod Dentofacial Res 7, no. 1 (2021): 62-67. https://doi.org/10.18231/j.ijodr.2021.011
